|
Dr Karen Anderson - Consultant Nephrologist
- The Richard Bright Renal Unit
- Southmead Hospital
- Bristol
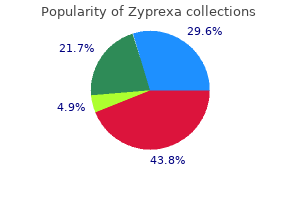
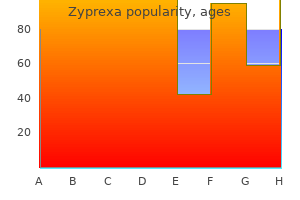
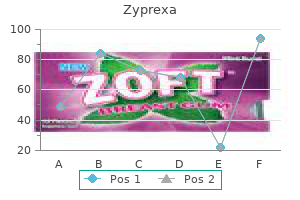
Zyprexa dosages: 20 mg, 10 mg, 7.5 mg, 5 mg, 2.5 mg
Zyprexa packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
5 mg zyprexa otcA lateral perspective of narrowed neuroforamen causing a lateral stenosis 14 Percutaneous Adhesiolysis 245 c L3 Spinous process Degenerative disc signs: height loss and protrusion L4 Facet joint: L4 inferior articular facet (hypertrophy) Foraminal narrowing L5 Nerve root Facet joint: L5 superior articular side (hypertrophy) medicine 968 order zyprexa 7.5mg mastercard. These compartments have been defined because the anterior, neuraxial, and posterior as proven in. Anterior view Atlas (C1) Axis (C2) Left lateral view Atlas (C1) Axis (C2) Cervical curvature Posterior view Atlas (C1) Axis (C2) Cervical vertebrae C7 T1 C7 C7 T1 T1 Thoracic curvature Thoracic vertebrae T12 L1 T12 L1 T12 L1 Lumbar vertebrae Lumbar curvature L5 L5 L5 Sacrum (S1�5) Sacrum (S1�5) Sacral curvature Coccyx Coccyx Coccyx Sacrum (S1�5). Reproduced Netter Medical Illustration used with permission of Elsevier) 14 Percutaneous Adhesiolysis 247 Anterior Fused factor Foramen transversarium 7 Cervical vertebrae Cervical vertebra 12 Thoracic vertebrae Rib Thoracic vertebra 5 Lumbar vertebrae Sacrum Fused element Coccyx Lumbar vertebra Posterior. It expands to 4�6 mm at its biggest width within the mid-lumbar spine and steadily decreases to about 3 mm on the S1 degree. There appears to be a paired nature to the ligament, with both proper and left portions. Anterior inside vertebral venous plexus Subarachnoid house Arachnoid mater Dura mater Posterior longitudinal ligament Position of spinal ganglion Posterior ramus Extradural space Extradural fat Anterior ramus Vertebral body Transverse course of Intervertebral disc Spinous process. Technical Aspects the technique of lumbar adhesiolysis includes accessing the lumbar epidural space either by utilizing a caudal, interlaminar, or transforaminal strategy. C1 spinal nerve exits above C1 vertebra Base of cranium Cervical enlargement C1 C2 C3 C4 C5 C6 C7 T1 T2 C1 C2 C3 C4 C5 C6 C7 C8 T1 C8 spinal nerve exits below C7 vertebra (there are eight cervical nerves however only 7 cervical vertebrae) Lumbar enlargement T2 T3 T3 T4 T4 T5 T5 T6 T6 T7 T7 T8 T8 T9 T9 T10 T10 T11 T11 T12 T12 L1 L1 L2 L3 L3 L2 Conus medullaris (termination of spinal cord) Internal terminal filum (pial part) Cauda equina L4 L4 L5 L5 Sacrum S1 External terminal filum (dural part) S2 S3 Termination of dural sac S4 S5 Coccygeal nerve Coccyx Cervical nerves Thoracic nerves Lumbar nerves Sacral and coccygeal nerves out by the injected fluid finding the weakest parts of the scar tissue. The increase of enough pressure from the injected volume can overflow into the adjoining compartment, thus demonstrating the compartmental filling precept, not mechanical lysis by the catheter [61]. Subsequently, a mix of local anesthetic and steroid is injected into the epidural space through the catheter, adopted by hypertonic saline neurolysis which is carried out by a gradual and intermittent injection of hypertonic saline, both by infusion or in incremental doses. Inject Omnipaque 240 and visualize unfold of distinction medium with caudal or lumbar epidurogram 3. After identification of the filling defect similar to the realm of the pain, thread a Racz catheter into the filling defect four. Inject further Omnipaque 240 to verify opening of the scar and unfold of injectate throughout the epidural space and nerve roots 5. After ascertaining for lack of motor blockade, inject 6 mL of 10% saline in two divided doses of 3 mL every, 15�30 min after injection of local anesthetic 2. Inject 6 mg of Celestone Soluspan or nonparticulate Celestone or 40 mg of alcohol-free Depo Medrol or alcohol-free 40 mg of triamcinolone 3. If ache occurs during infusion, it should be stopped, and additional 2�3 mL of local anesthetic is injected. Inject iohexol (Omnipaque 240) and visualize spread of contrast medium (epidurogram) three. If filling defect comparable to space of ache is current, thread Racz Tun-L-Kath (Epimed) catheter into filling defect (scar), while injecting normal saline via the catheter; observe fluoroscopically to visualize washout of contrast medium and opening of scar four. Inject additional iohexol to verify opening of scar and unfold of injectate throughout the epidural area 5. Inject preservative-free saline (2�20 mL) with or without hyaluronidase (Hylenex) 6. Tape catheter in place In the postoperative care unit: After ascertaining absence of motor blockade, inject 0. After the last therapy, remove the epidural catheter the procedure is repeated without steroids on day 2 and day three, whereas, within the Manchikanti technique, along with other modifications, the catheter is removed after performing the preliminary process. Racz Technique the approach employed by Racz and colleagues [5, 6, 10, 26, 37] is described as percutaneous epidural neuroplasty carried out under fluoroscopy. The Caudal Approach � the patient is positioned inclined with firm folded padding beneath the pelvis to straighten the lumbar backbone, with toes pointing inward. Fifteen hundred units of hyaluronidase in 10 mL of preservative-free saline is injected quickly. The trigger is normally the introduction of hypertonic saline into nonanesthetized epidural tissue. Fifteen minutes later, 10 mL of 10% saline is infused over 20 min for patient comfort. Interlaminar Lumbar Approach the method for lysing epidural adhesions on this area of the spinal twine have to be modified to be certain that the needle is 258. Five minutes later the remainder of the local anesthetic and steroid quantity is injected. Filling defects could be seen on lumbar epidurography at L5 and S1, adopted by adhesiolysis and acceptable nerve root filling seen within the posteroanterior view and ventral epidural filling seen in the lateral view. There is a scarcity of epidural filling and symptomatology indicating right L5 and S1 radiculitis. There is profitable adhesiolysis and nerve root filling post-adhesiolysis, along with ventral epidural filling on the lateral view. Excellent L5 nerve root filling is noticed, along with ventral filling seen on lateral epidurography. If no issues are observed and the affected person reviews good ache aid without any motor weak point, hypertonic saline neurolysis is carried out at this time by injecting variable doses of 10% sodium chloride resolution. Lateral view after adhesiolysis � An anteroposterior radiographic view of the sacral and lumbar epidural backbone exhibits an atypical epidural filling sample with no nerve roots and a non-areolar look. Subdural Placement � the subdural compartment lies between the dura mater and the arachnoid mater, extending from the lumbar backbone into the skull. Transforaminal Approach � When a lesion is inaccessible from the caudal house, a transforaminal strategy is made. One 2 mL of Omnipaque 240 is injected, and epidural spread is confirmed within the indirect, anteroposterior, and lateral views. When the above-described fluoroscopic rotations are carried out, the end plates find yourself being squared. The shadow of the spinal stenosis is seen secondary to the hypertrophic ligamentum flavum and the bulging L2 disc. Side Effects and Complications � the most common and worrisome problems of adhesiolysis in the lumbar backbone are related to dural puncture, spinal twine compression, catheter shearing, an infection, administration of steroids, hypertonic saline, and hyaluronidase [9, 26, 65�79]. Unintended subarachnoid or subdural puncture with injection of local anesthetic or hypertonic saline is likely considered one of the major problems of the procedure. Flexion and rotation of the head and neck can open up lateral runoff and release the stress by way of the enlarged neural foramina. Percutaneous adhesiolysis is carried out to eliminate the deleterious results of scar formation, assuring the focused supply of medicine or principally to provide the focused supply of drugs within the absence of scar formation. Post-lumbar laminectomy syndrome, or ache following operative procedures of the lumbar backbone, is estimated to occur in approximately 5�40% of sufferers after surgical intervention. Post-lumbar surgical procedure syndrome, spinal stenosis, and recalcitrant low back and decrease extremity ache secondary to disc herniation, radiculitis, or extreme degenerative disc disease are multifactorial issues with variable scientific presentations. Patients with chronic persistent pain that requires adhesiolysis may present with irritation, edema, fibrosis, and venous congestion; mechanical strain on posterior longitudinal ligaments, the annulus fibrosis, and spinal nerve; decreased or absent nutrient delivery to the spinal or nerve root; and central sensitization. One day lumbar epidural adhesiolysis and hypertonic saline neurolysis in remedy of persistent low back ache: a randomized, double-blind trial. Epidural neuroplasty versus physiotherapy to relieve pain in sufferers with sciatica: a prospective randomized blinded medical trial.
Buy generic zyprexa from indiaOnce current stroke treatment 60 minutes cheap zyprexa 5mg without a prescription, ache from the intervertebral disc persists in as much as 80% of patients [4]. On a physiologic basis, the event of tearing in the annulus, with subsequent neovascularization and progress of nerves from the outer annulus to the inside annulus and irritation of these nerves by inflammatory factors associated with healing, stays probably the most attractive speculation [6]. Alternative theories are that the warmth shrinks the collagen, inflicting it to reorganize and strengthen, or that granulation tissue is cauterized [7]. Fusion of the adjacent vertebral our bodies has commonly been used, with minimal profit for this analysis [9, 10]. Lumbar epidural injections provide important benefit in ache and performance in discogenic ache [11]. Various injection therapies, including ozone, methylene blue, and various biologic preparations, have been tried and show early promise [12�14]. Identifying the intervertebral disc because the supply of low back ache may be tough. History By the early Nineteen Nineties, there was considerable interest in the use of warmth to deal with discogenic low back ache. In 1993, Eric Cosman, who first conceptualized the application of radiofrequency vitality to generate warmth in tissues, and Menno Sluijter, who pioneered the scientific software of radiofrequency, utilized for a patent to use radiofrequency power applied to the nucleus, not the annulus, to treat low back pain [17]. Radiofrequency waves, between 250,000 and a 1,000,000 Hertz, cause ionic heating in the tissue instantly adjoining to the electrode. Tissue ablating heat is generated by ions moving in response to the radiofrequency electromagnetic field. This ionic activity causes both the tissue and the thermistor within the radiofrequency probe to warmth up [18]. They rejected radiofrequency as being unable, with then available know-how, to apply sufficient heat throughout the annulus to create the specified lesion. They rejected laser heat for lack of control and the risk to adjacent neural tissue. They chosen conductive heating, which is done by heating a wire, which transfers warmth to the fluids within the adjoining tissue, which in flip heats the goal tissue. Patient selection required failure of conservative therapy, ache restricted to the low back with no neurologic involvement of the decrease extremities, disc top of at least 50% of normal, and positive discography at a degree with a documented annular tear. The normal heating protocol was to enhance the temperature of the probe to 90� C over thirteen min and maintain the 90� temperature for four min. The monitor photographs and generator noises of an actual procedure have been then displayed, in order that the placebo patient had the identical intra-procedural experience as sufferers undergoing the procedure. Of the sixty four participants, eight have been excluded from that study for varied protocol violations. With a quantity wanted to treat of 5 to get a 75% reduction in scores, they concluded that it was a worthwhile intervention for chosen patients. At the tip of the procedure, all sufferers got one hundred mg of cefazolin intradiscally. Further, placebo effects are anticipated in studies; the absence of one raises methodological questions [36�38]. The introducer is positioned within the posterior annulus, using fluoroscopic and impedance monitoring, and the catheter is then passed alongside the posterior facet of the annulus as shown in. A lesion is then made using radiofrequency vitality applied over 10 min, with a maximum temperature of 65� C. Biacuplasty A limiting think about the usage of radiofrequency is that because the ionic heating of the tissues heats up the radiofrequency electrode, the tissue immediately adjoining to the electrode turns into heated, leading to charring, elevated impedance, and limitations on lesion measurement. Using water to cool the electrode prevents the charring adjacent to the electrode and allows a big lesion aspect. Both Pauza [42] and Petersohn sixteen Percutaneous Lumbar Thermal Annular Procedures 303. A bipolar lesion is made across the posterior annulus at 50 �C for 15 min adopted, without transferring the electrodes, by monopolar lesions at 60� for 2 min and 30 s. Inclusion standards have been low again ache unresponsive to conservative care, disc peak of a minimum of 50% and concordant discography in diseased discs with regular discography in management discs. They excluded sufferers with more than two involved levels or with a history of any previous lumbar spine surgery, disc bulges larger than 5 mm, or structural abnormalities corresponding to spondylolisthesis or central canal stenosis. They discovered six reviews of nerve root injury, 5 of which had been associated to the introducer needle placement. A separate report described a case of catheter shearing by which the catheter migrated from the annulus to the epidural area, causing nerve root irritation and necessitating surgical removal [47]. Discitis, osteonecrosis, and the event of grade 1 anterolisthesis have been reported [23, 50]. In one case, the catheter was placed in the vertebral foramen, a gross violation of ordinary of care, so that the cauda equina was instantly heated; within the second, the catheter was evidently appropriately placed [53]. The actual radiofrequency conductor containing the thermocouple (yellow) is accompanied by the cool water inlet (green) and outlet (red) (From Ball [18], with permission) eased, fissured annulus. The only complication reported with biacuplasty is the expected transient low back ache after needle insertion [54]. If the ache persists after conservative therapy, including remedy, train, oral and topical drugs, and epidural injection therapy, remedy options are restricted, and within the absence of different therapies, the situation is unlikely to enhance. Surgical procedures present uncertain outcomes and have important risks and morbidity, together with main decrements in perform. Isotherm traces kind dumbbell form round and between radiofrequency probes to cover the posterior section of the annulus fibrosus (Adapted from Kapural et al. Tearing of the annulus can result in decreased impedance with heat lesions extending to the region of the motor rootlets. Evidence-informed administration of continual low back pain with intradiscal electrothermal remedy. Intradiscal electrothermal remedy for persistent discogenic low again pain: a potential end result research with minimum 1-year follow-up. Systematic review of randomized trials evaluating lumbar fusion surgical procedure to nonoperative care for treatment of persistent back pain. Fusion surgical procedure for lumbar degenerative disc illness: still extra questions than solutions. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in chronic axial or discogenic low back ache: results of 2-year follow-up. Ozone therapy as a remedy for low back ache secondary to herniated disc: a scientific evaluation and meta-analysis of randomized managed trials. A randomized placebo-controlled trial of intradiscal methylene blue injection for the therapy of continual discogenic low again ache. Rejuvenation of nucleus pulposus cells using extracellular matrix deposited by synovium-derived stem cells. The science of typical and water-cooled monopolar lumbar radiofrequency rhizotomy: an electrical engineering perspective. Randomized controlled trial of percutaneous intradiscal radiofrequency thermocoagulation for chronic discogenic again pain: lack of effect from a 90-second 70 C lesion.
Discount 2.5mg zyprexa with mastercardInt J Surg Pathol 18: 48-54 MacCollum D W symptoms 8dpiui buy zyprexa 10mg free shipping, Martin L W 1956 Hemangiomas in infancy and childhood. Surg Clin North Am 36: 1647-1663 Watson W L, McCarthy W B 1940 Blood and lymph vessel tumors. Surg Gynecol Obstet seventy one: 569-588 Edgerton M T, Hiebert J M 1978 Vascular and lymphatic tumors in infancy, childhood and adulthood: challenge of prognosis and therapy. Arch Dermatol one hundred twenty: 1453-1455 Johnson S C, Hanke C W 2001 Unilateral acquired nevus flammeus in women. Pediatr Dermatol 26: 139-142 Adams B, Lucky A W 2000 Acquired port-wine stains and antecedent trauma: case report and evaluation of the literature. Hum Genet one hundred ten: 343-347 Askar I, Kilinc N, Yucetas A 2003 Pyogenic granuloma appearing on port-wine stain: a case report. J Eur Acad Dermatol Venereol 18: 238-239 Gautier-Smith P C, Sanders M D, Sanderson K V 1971 Ocular and nervous system involvement in angioma serpiginosum. Br J Ophthalmol 55: 433-443 Marriot P J, Munro D D, Ryan T 1975 Angioma serpiginosum- familial incidence. Br J Dermatol 93: 701-706 Johnson W C 1976 Pathology of cutaneous vascular tumors. Br J Dermatol a hundred and forty four: 363-368 Ishibashi A, Tsuboi R, Shinmei M 1984 -galactosidase and neuraminidase deficiency associated with angiokeratoma corporis diffusum. Acta Dermat Venereol 41: 56-60 Imperial R, Helwig E B 1967 Angiokeratoma of the scrotum (Fordyce type). Obstet Gynecol 29: 307-312 Lynch P J, Kosanovich N 1967 Angiokeratoma circumscriptum. Acta Derm Venereol 49: 386-389 Coffin C M, Dehner L P 1993 Vascular tumors in children and adolescents: a clinicopathologic examine of 228 tumors in 222 sufferers. Lancet 1: 1429-1434 Boon L M, Enjolras O, Mulliken J B 1996 Congenital hemangioma: evidence of accelerated involution. Plast Reconstr Surg 107: 1647-1654 Mulliken J B, Enjolras O 2004 Congenital hemangiomas and infantile hemangioma: missing hyperlinks. J Am Acad Dermatol 50: 875-882 Perrone T 1985 Vessel-nerve intermingling in benign infantile hemangioendothelioma. Cancer 43: 2322-2331 Gonzalez-Crussi F, Reyes-Mugica M 1991 Cellular hemangiomas ("hemangioendotheliomas") in infants. Am J Surg Pathol 15: 769-778 Smoller B R, Apfelberg D B 1993 Infantile (juvenile) capillary hemangioma: a tumor of heterogeneous mobile parts. Clinical options, incidence, histology and results of therapy: report of 242 instances. Patrice S J, Wiss K, Mulliken J B 1991 Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic research of 178 cases. Ogunleye A O, Nwaorgu O G 2000 Pyogenic granuloma, a reason for congenital nasal mass: case report. Willies-Jacobo L J, Isaacs H Jr, Stein M T 2000 Pyogenic granuloma presenting as a congenital epulis. Nappi O, Wick M R 1986 Disseminated lobular capillary hemangioma (pyogenic granuloma). Wilson B B, Greer K E, Cooper P H 1989 Eruptive disseminated lobular capillary hemangioma (pyogenic granuloma). Palmero M L, Pope E 2009 Eruptive pyogenic granuloma growing after drug hypersensitivity reaction. Warner J, Wilson-Jones E 1968 Pyogenic granuloma recurring with a number of satellites. Tursen U, Demirkan F, Ikizoglu G 2004 Giant recurrent pyogenic granuloma on the face with satellitosis conscious of systemic steroids. Piguet V, Borradori L 2002 Pyogenic granuloma-like lesions during capecitabine therapy. MacKenzie-Wood A R, Wood G 1998 Pyogenic granuloma-like lesions in a affected person utilizing topical tretinoin. Exner J H, Dahod S, Pochi P E 1983 Pyogenic granuloma-like acne lesions throughout isotretinoin therapy. Padilla R S, Orkin M, Rosai J 1987 Acquired "tufted" angioma (progressive capillary hemangioma). Herron M D, Coffin C M, Vanderhooft S L 2002 Tufted angiomas: variability of scientific morphology. Ramesh R, De Silva B, Atherton D J 2009 Congenital tufted angioma with persistent low-grade coagulopathy. Chu C Y, Hsiao C H, Chiu H C 2003 Transformation between Kaposiform hemangioendothelioma and tufted angioma. Slater L N, Welch D F, Min K W 1992 Rochalimaea henselae causes bacillary angiomatosis and peliosis hepatis. Girard C, Graham J H, Johnson W C 1974 Arteriovenous hemangioma (arteriovenous shunt): a clinicopathologic and histochemical study. Akiyama M, Inamoto N 2001 Arteriovenous haemangioma in persistent liver disease: medical and histopathological features in four circumstances. Koutlas I G, Jessurun J 1994 Arteriovenous hemangioma: clinicopathological and immunohistochemical research. Mentzel T, Partanen T A, Kutzner H 1999 Hobnail hemangioma ("targetoid hemosiderotic hemangioma"): clinicopathologic and immunohistochemical analysis of 62 circumstances. Christenson L J, Stone M S 2001 Trauma-induced simulator of targetoid hemosiderotic hemangioma. Carlson J A, Daulad S, Godheart H P 1999 Targetoid hemosiderotic hemangioma-a dynamic vascular tumor: report of 3 cases 83 166. J Cutan Pathol 29: 154-158 Requena L, Kutzner H, Mentzel T 2002 Acquired elastotic hemangioma: a clinicopathologic variant of hemangioma. Am J Dermatopathol 30: 16-20 Wells G C, Whimster I W 1969 Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol 81: 1-15 Wilson-Jones E, Bleehen S S 1969 Inflammatory angiomatous nodules with irregular blood vessels occurring concerning the ears and scalp (pseudo or atypical pyogenic granuloma). Arch Dermatol 102: 422-427 Rosai J, Akerman L R 1974 Intravenous atypical vascular proliferation. Arch Dermatol 109: 714-717 Rosai J, Gold J, Landy R 1979 the histiocytoid hemangiomas. A unifying concept embracing several beforehand described entities of skin, gentle tissue, large vessels, bone and heart. Hum Pathol 10: 707-730 Cooper P H 1988 Is histiocytoid hemangioma a specific pathologic entity Am J Surg Pathol 12: 815-817 Rosai J 1982 Angiolymphoid hyperplasia with eosinophilia of the pores and skin. Am J Dermatopathol four: 175-184 Allen P W, Ramakrishna B, MacCormac L B 1992 the histiocytoid hemangiomas and different controversies. Histol Histopathol eight: 187-212 Fetsch J F, Weiss S W 1991 Observations in regards to the pathogenesis of epithelioid hemangioma (angiolymphoid hyperplasia). Mod Pathol four: 449-455 Olsen T G, Helwig E B 1985 Angiolymphoid hyperplasia with eosinophilia. J Am Acad Dermatol 12: 781-796 Castro C, Winkelmann R K 1974 Angiolymphoid hyperplasia with eosinophilia in the skin.
Purchase zyprexa cheap onlineProvocation pertains to the combined procedure medications for ptsd purchase zyprexa 7.5mg with amex, in which the disc is stimulated but an image of the disc is also obtained. In distinction, discography is a process by which photographs of the disc are obtained irrespective of whether or not ache is reproduced or not [4]. In current years, the use of anesthetic discography has generated important curiosity as a way to reduce the excessive falseL. Anesthetic discography is used as either an adjunct or replacement of provocation discography; whether it enhances the accuracy of the diagnosis is debated [1, 4]. History the lumbar disc was not thought-about an important reason for low again pain or radiculopathy until Mixter and Barr in 1934 [10] reported the surgical removing of a posterior disc prolapse resulting in relief of these symptoms. In 1940, Roofe [11] ascertained the nerve provide to the annulus that laid down a basis for understanding that the intervertebral disc alone might be a ache generator. Lindblom [12], in 1944, revealed the existence of annular pathology throughout the cadaveric discs after injecting purple dye into the disc nucleus that extended into annular tears. Hirsch [13] famous in 1948 that the injection of procaine into the lumbar disc provided pain relief confirming that the disc was a supply for axial low back ache. Subsequently, Lindblom [14], in 1948, reported the clinical use of lumbar disc injections to identify disc(s) liable for low back ache and sciatica. Cloward [15] and Smith and Robinson [16] initially pioneered cervical discography and in 1958 separately printed papers relating to cervical discography within the evaluation of persistent neck ache, headache, and shoulder ache. Holt [17] later published a report in 1964 that brought into question the validity and function of cervical discography. In 1969, Klafta and Collis [18, 19] studied cervical discography and concluded that a cervical disc injection inflicting significant pain was probably due to an abnormal disc. Thoracic discography was not carried out as a diagnostic device until approximately 30 years after lumbar discography. In 1975, Simmons and Segil [25] described thoracic discography and nucleography in the evaluation of a man with mid-thoracic radicular ache. Of all of the interventional diagnostic tests, provocation discography is the only take a look at that depends on replica of ache, instead of reduction of pain by native anesthesia. However, there has been significant concern that analgesic discography has a high false-negative price, which has been debated [29]. Analgesic discography has been gaining popularity, and a number of protocols have been developed [29�32]. However, the controversy surrounding discography continues to improve, and the place of discography within the management of painful spinal circumstances continues to emerge. The regular getting older and degeneration of the intervertebral disc is intently related to the number of vessels that attain the intervertebral disc, especially the cartilaginous endplate. As the variety of vessels lower and the nutrition offered and waste eliminated by these vessels decrease, the changes related to intervertebral disc growing older and degeneration increase [33]. The number of clefts and radial tears increases from 17 to 20 years of age and the overall variety of chondrocytes decreases as cell demise, mucoid degeneration, and granular changes begin to appear [28]. Pain compression both contribute caused by mechanical forces superimposed to lumbar pain on chemically activated nociceptors Disc Rupture and Nuclear Herniation Herniated Nucleus Pulposus Neovascularization of disc Inflammatory cell infiltrate (chemical signal for revascularization) 275 Nucleus pulposus Phospholipase A2 Prostaglandins Nitric oxide Metalloproteinases Unidentified inflammatory Rim lesion Nucleus pulposus Tears in internal annular lamellae Shortened disc space Herniated nucleus pulposus Peripheral tear of annulus fibrosus and cartilage end plate (rim lesion) initiates sequence of occasions that weaken and tear inner annular lamellae, permitting extrusion and herniation of nucleus pulposus. Rationale Rationale for lumbar discography has been nicely studied with some literature on cervical discography, whereas with very scant literature on thoracic discography. Validity � Examination of cadaver discs typically confirms the presence of annular tears and disc degeneration, as revealed by discograms [1, 4, 5]. Evidence Base Evidence of effectiveness is set based mostly on greatest proof synthesis starting from Level I to V with Level I evidence being the highest stage of proof obtained from multiple high-quality diagnostic accuracy studies [87]. Thoracic discography is beneficial to resolve if an intervertebral disc is painful or not in rare circumstances. Indications � Unremitting spinal pain, with or without extremity ache, of larger than three months length. In these circumstances, discography will be the only study capable of providing a diagnosis or allowing a precise description of the inner anatomy of the disc. The mobile part of the backbone contains 7 cervical, 12 thoracic, and 5 lumbar vertebrae, whereas inflexible sacrum which offers a relatively inflexible connection to the innominate bones is shaped by 5 fused vertebrae. Each intervertebral disc consists of an annulus fibrosus, an outer fibrous half, composed of concentric lamellae of fibrocartilage and a gelatinous central mass referred to as the nucleus pulposus. Anatomy � the vertebral column is flexible because it consists of many vertebrae which are separated by resilient intervertebral discs. The 25 cervical, thoracic, lumbar, and first sacral vertebrae also articulate at synovial zygapophyseal joints. Technical Aspects Among the discography carried out in the cervical, thoracic, and lumbar areas, lumbar discography is probably the most studied and published. Lumbar Discography � the two techniques which have been used for lumbar discography are the transdural and extraspinal approaches. Notice the parts of the intervertebral disc: annulus fibrosus, nucleus pulposus, and vertebral (cartilaginous) endplate. Disc Injection � Regardless of the method, after the needles are positioned in the disc(s), each disc is evaluated by injecting saline or distinction, or both, in sequence. Lumbar intradiscal pressure can be immediately measured with a stress gauge in kilos per sq. inch (psi) at the onset of pain or with a agency endpoint. The pain stage is a mirrored image of the ache depth skilled by the patient in the course of the injection regardless if the pain is similar or not (concordant or discordant). The ache high quality is most necessary since it establishes whether or not or not pain produced during the process is exactly what the patient clinically experiences. Cervical Discography Cervical discography may be performed using an authentic anterior strategy or modified anterolateral approach. However, anterolateral approach is the most commonly utilized method associated with less danger. Anterior Approach � the original anterior approach for performing cervical discography entails placing the affected person within the supine position. Intravenous antibiotics and lightweight intravenous sedation is given to the patient previous to starting the process. This figure illustrates needle placement into L3/4, L4/5 and L5/S1 disc areas with an oblique strategy 284 L. Anterolateral Approach � the anterolateral method for cervical discography positions the affected person in supine with positioning the fluoroscope obliquely for an optimum view of the foramen at the meant disc level. Disc Injection � Each disc is evaluated by injecting either saline or contrast, or each, in sequence after the needles are positioned in the discs. Thoracic Discography the strategy of thoracic discography is much like lumbar discography. However, extraspinal method is the recommended approach, which is secure contemplating the location of the spinal wire within the thoracic backbone. Disc Entry � An extraspinal technique much like that used for lumbar discography is utilized in performing thoracic discography.
Buy 5 mg zyprexa overnight deliveryKaposiform hemangioendothelioma may be distinguished from angiosarcoma by its lack of cytologic atypia and the absence of individually infiltrative treatment croup purchase zyprexa online now, anastomosing channels. It presents as a slowly rising cutaneous tumor, most frequently in younger adults; no sex predominance is seen. Very not often, these lesions can come up after radiotherapy or within the setting of chronic lymphedema. This appearance is conferred by the presence of elongated, arborizing blood vessels. A prominent stromal and intraluminal lymphocytic infiltrate is present in maybe 50% of circumstances. These endothelial cells have limited, usually basal, cytoplasm, and vacuolation is uncommon. The vascular lumina may contain occasional papillae with hyaline collagenous cores. Most tumors present focally strong areas composed of monomorphic spindle or epithelioid cells, which often stain positively for endothelial markers. Recently, nonetheless, follow-up in eight of 12 reported circumstances revealed neither native recurrences nor metastatic spread. Therefore the issue in regards to the true malignant potential of this tumor will remain unsolved until additional collection are reported. Hobnail hemangioma occurs primarily in youngsters and young adults and in a wide range of anatomic sites, including the oral cavity. Histologically, the lesions are inclined to be superficial and circumscribed, with a sparse inflammatory infiltrate and solely focal hobnail endothelial cells. Angiosarcoma normally occurs in a different scientific setting and is characterized by irregularly infiltrative vascular channels, lined by atypical endothelial cells, which usually present multilayering. Histologic Appearances Using stringent diagnostic criteria, our experience and that of others255 counsel that these tumors are often composed of dilated, irregular vascular channels resembling a cavernous lymphangioma, although some cases have smaller, irregularly branching vascular channels. Numerous lymphocytes are seen not solely within the surrounding stroma but also within the vascular channels. The endothelial cells lining some of the areas have a prominent atypical nucleus and inconspicuous cytoplasm, giving a typical hobnail or matchstick appearance. Most characteristic is the presence of prominent endothelial intraluminal papillary tufts. These hyaline cores appear to be composed of basement membrane materials synthesized by the tumor cells. More than 50% of patients have a number of nodules, often involving a number of tissue planes in the identical basic anatomic region-most usually skin, subcutis, and skeletal muscle and fewer usually bone. Despite this very worrisome presentation, metastasis appears to be very infrequent. Limited genetic knowledge have shown that these lesions have a t(7;19)(q11;q13) translocation. Cavernous lymphatic-like areas contain prominent endothelial papillae and clusters of lymphocytes. The most frequent differential diagnosis is epithelioid sarcoma, but the latter is generally not dominated by myoid-appearing spindle cells. Although the cell of origin remains controversial, most proof points towards endothelial cells, significantly lymphatic endothelium, because the principal mobile component272-276; increasingly, nevertheless, it would seem that these lesions comprise a mixed-cell population. For many years epidemiologic and clinicopathologic findings advised that an etiologic association with an infectious organism was probably, and various other viral organisms, including cytomegalovirus, were initially implicated as the culprit. Histologically, composite hemangioendothelioma usually consists of admixed components of benign, intermediate, and morphologically malignant vascular components. Many circumstances even have areas indistinguishable from low-grade angiosarcoma (which, in other circumstances, may need heralded more aggressive behavior), and some examples moreover show options of spindle cell hemangioma. In circumstances with a benign component, areas with features of a lymphangioma may be seen. Prolonged follow-up has revealed its ability to metastasize and to pursue a deadly scientific course, suggesting that it could in reality represent an unusual variant of angiosarcoma. Histologically it consists of an unusual admixture of stable, angiomatous, and primitive vascular patterns. Histologic Appearances Regardless of the scientific subgroup, all instances show related histologic features. Three distinctive levels, which may overlap, are described based on the evolution of a specific lesion: patch, plaque, and nodular stage. Early modifications in the patch stage can be very subtle: confusion with an inflammatory dermatosis is feasible. In the reticular dermis, particularly close to the surface and round preexisting blood vessels and adnexal structures, a proliferation of irregular, small, jagged vascular channels is seen, lined by a single layer of mildly atypical endothelial cells. Surrounding these vessels are extravasated purple blood cells related to hemosiderin deposition and a sparse inflammatory infiltrate composed of lymphocytes and plasma cells. Normal blood vessels and adnexal buildings could protrude into the neoformed blood vessels in a trend described because the promontorysign. Focally, typically putting collagen dissection is seen, similar to that in angiosarcoma. The plaque stage represents an exaggeration of the patch stage with involvement of the whole reticular dermis and even the subcutis. The spindle cell element is more pronounced, and hemosiderin deposition becomes extra outstanding. Extensive patch and plaque disease in a young homosexual male with acquired immunodeficiency syndrome. Regression of lesions is usually seen after withdrawal or reduction of immunosuppression. Numerous jagged vascular spaces dissect by way of the dermis and around pores and skin adnexa. The vascular channels are probably to be parallel to the dermis (A) and are commonly related to extravasated purple blood cells, plasma cells, and hemosiderin deposition (B). Between the spindle cells are numerous slit-like vascular areas containing extravasated purple blood cells. Associations embody cryptococcosis, tuberculosis, and Mycobacterium avium intracellulare. Differential Diagnosis Histologically, the differential diagnosis includes benign lymphangioendothelioma, hobnail hemangioma, spindle cell hemangioma, kaposiform hemangioendothelioma, cutaneous angiosarcoma, acroangiodermatitis, aneurysmal benign fibrous histiocytoma, and so-called multinucleate cell angiohistiocytoma. Aneurysmal benign fibrous histiocytoma is more polymorphic with foam cells, multinucleate giant cells, and absence of vascular clefts. Features of acroangiodermatitis314 comprise proliferation of small blood vessels of the superficial vascular plexus, commonly in a nodular arrangement, accompanied by fibrosis, hemosiderin deposition, and only a few inflammatory cells.
Gamma-Linolenic Acid (Gamma Linolenic Acid). Zyprexa. - Dosing considerations for Gamma Linolenic Acid.
- Are there safety concerns?
- Breast cancer, oral polyps, hyperlipidemia (high cholesterol and blood fat levels), heart disease, cancer prevention, attention deficit-hyperactivity disorder (ADHD), depression, chronic fatigue syndrome, hayfever, psoriasis, eczema, and other conditions.
- Allergic skin conditions (eczema).
- High blood pressure.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96782
Buy discount zyprexa 2.5 mg on lineIf no additional epidural (intravascular treatment 2nd degree burn discount 7.5 mg zyprexa with mastercard, subarachnoid, or gentle tissue) distinction pattern is appreciated with adverse aspiration with 3�5 mL of distinction, an injectate of local anesthetic, preservative-free lidocaine zero. The "railroad observe" appearance is attribute of epidural localization of the contrast. Contrast injection will reveal subarachnoid patterns: � Contrast is also injected to perform myelograms. This house accommodates solely a small volume of serous fluid between opposing membranes [63, 64]. Most commonly, posterior subdural injections are carried out, but anterior subdural injections may be carried out. The diploma of effects depends on the extent of subdural compartmentalization and the volume injected: � Injection into the anterior subdural area could also be related to excessive motor and sensory blocks and even lack of consciousness [65], whereas posterior subdural injection often presents as a failed spinal block or a patchy epidural block of slow onset, requiring massive volumes of local anesthetic for correction. The posterior border of the fluid collection is linear (dura mater), while the anterior border is somewhat more irregular in the arachnoid mater. Thoracic Transforaminal Epidural Injections � Thoracic transforaminal epidural injections are carried out infrequently. Critical Anatomy � the spinal branches are the principle arteries of supply to all bony elements of the vertebra and to the dura and epidural tissues; in addition they contribute to the availability of the spinal twine and nerve roots via radicular branches. Posterior spinal arteries Anterior spinal artery Anterior segmental medullary artery Anterior radicular artery Posterior radicular artery Branch to vertebral physique and dura mater Spinal branch Dorsal branch of posterior intercostal artery Posterior intercostal artery Paravertebral anastomoses Prevertebral anastomoses Thoracic (descending) aorta Section through thoracic level: anterosuperior view Sulcal (central) branches to right facet of spinal cord Posterior radicular artery Anterior segmental medullary artery Pial arterial plexus Anterior and posterior radicular arteries Anterior spinal artery Right posterior spinal artery Peripheral branches from pial plexus Sulcal (central) branches to left facet of spinal wire Left posterior spinal artery Posterior radicular artery Arterial distribution: schema Anterior segmental medullary artery Pial arterial plexus Note: All spinal nerve roots have associated radicular or segmental medullary arteries. Reproduced Netter Medical Illustration used with permission of Elsevier) 12 Thoracic Epidural Injections 201 � Each artery divides into a sequence of main branches (abdominal wall, intermediate or spinal canal, and the posterior body wall branches) just outdoors the extent of the intervertebral foramina. Care have to be taken to perform procedures in a fashion which minimizes the chance of the needle or instrument encountering the artery. Technical Implications � Thoracic transforaminal epidural injection procedures could additionally be carried out much like lumbar. Supraneural has been described as the safe triangle method within the thoracic and lumbar backbone: � Thoracic transforaminal injections share multiple risks much like cervical and lumbar transforaminal epidural injections with basic antagonistic results associated to placing a needle into an intervertebral foramen, with important neurovascular issues, together with additional issues related to puncturing the lung. They also assume an artery could be entered and dye and/or native anesthetic injected after which exited with out native sequelae secondary to injury to the artery. The native anesthetic test dose suffers from issue in measuring outcomes parameters. These mechanisms are local phenomena based mostly on penetration and damage to the artery itself. These embrace intimal flaps, vasospasm, thrombosis, and transection of the artery. Of note, the outer diameters of the artery in the foramen and a 22 g needle are quite related. There now may be angiographic evidence of obstruction to circulate through an injured radiculomedullary artery following a right L2�3 transforaminal epidural steroid injection [79]. Supraneural Approach � Supraneural approach has been generally used with indirect or posterior method: � For the posterior method, the patient is placed within the susceptible position with a firm padding underneath the chest, and the fluoroscopy unit is positioned with the spinous process in the middle of the backbone. A small volume of distinction is injected, and the sample of dispersion into the nerve root is famous: � If the needle has penetrated the epiradicular membrane surrounding the nerve root, an acceptable and optimistic image of the nerve root might be seen on fluoroscopy with acceptable dispersion of the distinction. If paresthesia is noticed, the needle must be withdrawn roughly a millimeter or so, and distinction is injected. Infraneural Approach � the procedure utilizing infraneural approach may be performed either with posterior or indirect approach: � Atluri et al. Observing the needle place in posterior or in lateral views, with injection of a small quantity of distinction, the pattern of dispersion into the nerve root is famous: � If the needle has penetrated the epiradicular membrane surrounding the nerve root, an acceptable and positive picture of the nerve root might be seen on fluoroscopy, with appropriate dispersion of the distinction, as proven in. After unfavorable aspiration for blood and cerebrospinal fluid and also negative vascular and intrathecal/subdural distinction unfold, inject the treatment. Side Effects and Complications � Potential problems of thoracic spinal injections embody dural puncture, an infection, vascular/neurological damage, and results related to drug administration (Table 12. Multiple causes described for persistent thoracic and chest wall pain embody disc herniation, discogenic pain, post-thoracic laminectomy syndrome, and spinal stenosis. Thoracic epidural injections are administered with two approaches, particularly, interlaminar and transforaminal, with each approaches related to sure advantages and risks. Anatomically, the angulation is gentle from T1 to T4 and T9 to T12, whereas angulation is extra marked downward from T5 to T8, influencing the convenience of entry into the epidural space, with increased technical issue between T5 and T8. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and traits as detected by computed tomography after myelography. Safeguards to forestall neurologic problems after epidural steroid injections: evaluation of proof and lack of applicability of controversial policies. The complications related to needle placement embrace an infection, hematoma formation, abscess formation, subdural injection, intracranial air injection, nerve harm, intravascular injection, vascular damage, spinal cord ischemia, paralysis, pneumothorax, and cerebral vascular or pulmonary embolus. Multiple precautions should be exercised with application of risk reduction strategies in performing transforaminal epidural injections. Acknowledgments this e-book chapter is modified and up to date from a earlier book chapter, "Thoracic Interlaminar Epidural Steroid Injections" by Kenneth P. Immediate issues and pain reduction related to 296 fluoroscopically guided thoracic foraminal nerve blocks. Thoracic interlaminar epidural injections in managing continual thoracic ache: a randomized, double-blind, controlled trial with a 2-year follow-up. Spinal cord stimulation for therapy of ache in a affected person with submit thoracotomy pain syndrome. Comparative study of the azygous venous system in man, monkey, canine, cat, rat and rabbit. The dorsomedian connective tissue band in the lumbar epidural space of humans: an anatomical research using epiduroscopy in autopsy cases. Assessing the prevalence of saline versus air to be used within the epidural loss-of-resistance technique: a literature review. Accidental subdural injection during tried lumbar epidural block may present as a failed or inadequate block: radiographic evidence. Needle place analysis in cases of paralysis from transforaminal epidurals: consider various approaches to conventional strategies. Valor de la aspiracion liquada en al espacio peridural en la anesthesia peridural. Effects of steroids and lipopolysaccharide on spontaneous resorption of herniated intervertebral discs. Local corticosteroid utility blocks transmission in normal nociceptive C-fibers. The effect of epidural injection of betamethasone or bupivacaine in a rat mannequin of lumbar radiculopathy. Foundations of ache medication and interventional pain management: a comprehensive evaluation.
Cheap zyprexa 10mg on lineUnlike mounted sutures symptoms zoloft overdose order zyprexa 5mg without prescription, the adjustable suture technique allows modification of the place of the muscle. An adjustable suture includes quickly positioning the muscle, but not finally tying it down till the patient is awake and has been remeasured. After the affected person is freed from the consequences of anesthesia, measurements are retaken, and the muscle is positioned in its optimum position, to correctly align the eyes, after which securely tied down. Adjustable strabismus surgery ideally reduces the frequency of reoperations by eliminating undesirable early postop undercorrections or overcorrections and will increase the speed of surgical success. Both topical and peribulbar anesthesia have the benefit of providing good akinesia and anesthesia however with out the dangers associated with a retrobulbar injection. When using topical anesthesia, this may be augmented by means of minimal sedation and/or antianxiety drugs. Most children might be healthy, but the affiliation of strabismus with cerebral palsy, prematurity, and craniofacial and neurological disorders requires careful preop evaluation. At one time, it was believed that kids undergoing strabismus surgery had been at elevated threat for malignant hyperthermia. Although this has been shown to be inaccurate, many neuromuscular syndromes are associated with musculoskeletal abnormalities including strabismus and ptosis. Anninger W, Forbes B, Quinn G, et al: the impact of topical tetracaine eye drops on emergence behavior and pain aid after strabismus surgical procedure. Aouad M, Yazbeck-Karam V, Nasr V, et al: A single dose of propofol at the end of surgery for prevention of emergence agitation in children present process strabismus surgery during sevoflurane anesthesia. Hahnenkamp K, Honeman C, Fischer L, et al: Effect of different anesthetics on the oculocardiac reflex during pediatric strabismus surgical procedure. Keaney A, Diviney D, Harte S, et al: Postoperative behavioral changes following anesthesia with sevoflurane. Madan R, Bhatia A, Chakithandy S, et al: Prophylactic dexamethasone for postoperative nausea and vomiting in pediatric strabismus surgical procedure: dose ranging and safety analysis study. Min S-W, Hwang J-M: the incidence of asystole in sufferers undergoing strabismus surgery. Mizrak A, Erbagci I, Arici T, et al: Dexmedetomidine use throughout strabismus surgery in agitated youngsters. Seo I-S, Seong C-R, Jung G, et al: the impact of sub-Tenon lidocaine injection on emergence agitation after basic anesthesia in pediatric strabismus surgical procedure. As with any surgical procedure, preop education of the widespread risks must be discussed with the family and understood by all members of the affected person care group. If the affected person is a mature, cooperative adolescent (without claustrophobia) present process longer laser procedures. The needle is launched along the inferior orbital rim 1/3 of the means in which from the lateral orbital rim, aspirated to guarantee proper placement, and then the anesthetic is run at the appropriate quantity for the patient age, weight, and gender (usually ~5 mL). Communication and teamwork are essential to optimize the surgical experience for all. Laser photocoagulation may be performed at the side of different vitreoretinal procedures, corresponding to vitrectomy (described in laser section), intravitreal injection, and fluorescein angiography. Procedure: Laser photocoagulation takes advantage of the spatial precision offered by collimated light vitality to selectively (to the extent of cells) ablate pathologic tissues-usually retina. When the laser is focused at an ocular structure, the tissue absorbs the sunshine energy and generates warmth, and the surgeon can photocoagulate the aberrant tissue while minimally damaging other structures. The surgeon makes use of an indirect ophthalmoscope with a condensing lens to deal with the fundus. Two procedures commonly accompany laser photocoagulation: intravitreal injection and fluorescein angiography. This is most often performed for vascular proliferative retinopathy secondary to retina ischemia. Fluorescein angiography could also be used to identify ischemic areas of retina for panretinal or scattered photocoagulation. Intravenous injection of fluorescein carries the dye to the retina and choroidal circulation within seconds, and thus, the ophthalmologist can visualize perfusion of the choroids and retina over the subsequent 5�15 min. The anesthesiologist is normally asked to perform the iv fluorescein push while the retina physician operates the camera. The potential complications for laser photocoagulation include inadvertent irradiation of other, usually extra anterior, ocular constructions such as the cornea, iris, lens, and so forth. Vitrectomy in a toddler under 1 yr of age is essentially the most troublesome and least forgiving surgical procedure in ophthalmology. In older youngsters with complicated retinal detachments, typically the process takes from 45 to 75 min. Traumatic and/or rhegmatogenous retinal detachment instances, often in older kids, are often accompanied by a scleral buckle process, which entails isolating and manipulating the 4 recti muscular tissues. Procedure: After ensuring the eye is fully anesthetized and sterilized, the ophthalmologist creates a three-point sclerotomy with 23- or 25-gauge incisions through the pars plana, which is positioned 3�4 mm from the limbus (in a toddler larger than 2 yr; in younger youngsters, pars plicata incisions may be made 1 mm posterior to the limbus), on the inferotemporal, superonasal, and supertemporal locations. At the inferotemporal post an infusion cannula maintains the stress of the eye by allowing saline to exchange the excised tissue. The different two ports are then used for the instrumentation necessary to perform a bimanual vitrectomy. One of these instruments has a light hooked up to preserve visualization of the retina throughout the process. The surgical microscope and a wide-angle viewing system are used to perform the operation. To take away the precise vitreous substance, the posterior hyaloid is rigorously elevated and reduce with a microvitrectomy hand piece that simultaneously aspirates vitreous parts. The core vitrectomy is then performed for all 360� of the globe, using all surgical ports as necessary. Silicone oil could also be slowly infused into the posterior portion of the eye to substitute the removed vitreous. A subconjuctival injection of an antibiotic (usually cefazolin) and steroid (decadron) is then administered. Otherwise, if a buckle is current, a complex vitrectomy with attainable diathermy, lens removing, iridectomy, retinectomy, perfluoron, laser, and silicone oil could additionally be wanted. Laser therapy is instituted based mostly on the world and severity of retinal vascular proliferation in an try to stop loss of visual acuity or retinal detachment. These infants are at greater danger for perioperative issues than are older youngsters. Even in the toddler requiring no supplemental oxygen preop, managed ventilation could also be necessary even after minor surgical intervention. For term or older infants presenting from house, postop inpatient apnea monitoring is really helpful prior to forty eight wk postgestational age. For infants with comorbidity or prematurity, consider inpatient admission for these less than 52�60 wk postgestational age. An initial examination under anesthesia is often performed to determine the necessity for surgical intervention. Mask anesthesia can allow for a superb examination with consideration to obtaining a deep enough airplane for the eyes to return to midline rather than "sundowning" or being disconjugate.
Buy discount zyprexa 10mg lineIf not treatment advocacy center discount zyprexa 10mg with mastercard, the chance of the needle placement in the midzone of the foramen will increase. Although typically medial contrast unfold could be achieved within the posterior part of the foramen, sometimes the needle could need to be advanced to the anterior part of the foramen. Extraneural Placement of Needle � Intravascular placement of the needles with transforaminal epidural injections is way higher than lumbar interlaminar and caudal epidural injections [62, eighty, 81]. The range of intravascular penetration in the lumbosacral area has been proven to be as excessive as 15% at lumbar ranges and 46% at sacral levels. Caudal epidural injections must be performed with eleven Lumbar Epidural Injections a hundred seventy five. Failure to use fluoroscopy increases the prevalence of extra-epidural placement of the needle and injections [1, 86]. However, occasional issues may turn out to be worrisome specifically with transforaminal epidural 180 L. Precautions � Relative contraindications to interventional strategies, specifically epidural injections, have been described in patients receiving therapy with antithrombotics and anticoagulants [1, 88, 89, 95�101]. There are multiple causes described for chronic low back and decrease extremity pain that embrace disc herniation, discogenic pain, post-lumbar laminectomy syndrome, and spinal stenosis. Lumbar epidural injections are administered with three approaches, namely, caudal, interlaminar, and transforaminal. The emerging evidence shows lack of serious distinction between local anesthetic alone and with steroids, specifically in spinal stenosis, discogenic pain, and postsurgery syndrome, with somewhat superior results with steroids in disc herniation. The issues associated to needle placement embody an infection, hematoma formation, abscess formation, subdural injection, intracranial air injection, nerve injury, intravascular injection, vascular injury, spinal twine ischemia, paralysis, and cerebral vascular or pulmonary embolus. Anticoagulant therapy should be carefully balanced contemplating the high threat of thromboembolic phenomenon related to bleeding complications. Do epidural injections provide short- and long-term reduction for lumbar disc herniation R�sultats favorables m�me dans les cas chroniues par la coca�ne � doses �lev�es et r�p�t�es � intervalles raproches. Intractable sciatica-the sacral epidural injection- an effective technique of giving pain relief. Painful radiculopathy treated with epidural injections of procaine and hydrocortisone acetate: leads to 113 sufferers. Report of working get together on epidural use of steroids within the administration of again pain National Health and Medical Research Council. Epidural corticosteroid injections within the management of sciatica: a systematic evaluation and meta-analysis. Efficacy of epidural injections in the remedy of lumbar central spinal stenosis: a scientific evaluation. The tissue origin of low again pain and sciatica: a report of ache response to tissue stimulation during operation on the lumbar spine utilizing local anesthesia. Epidural injections for lumbar radiculopathy and spinal stenosis: A comparative systematic evaluate and meta-analysis. The prevalence and scientific options of inner disc disruption in patients with continual low again ache. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. A randomized, double-blind managed trial of lumbar interlaminar epidural injections in central spinal stenosis: 2-year follow-up. Fluoroscopic caudal epidural injections in managing post lumbar surgical procedure syndrome: twoyear outcomes of a randomized, double-blind, active-control trial. Effect of caudal epidural steroid or saline injection in continual lumbar radiculopathy: multicentre, blinded, randomised controlled trial. Transforaminal versus interlaminar approaches to epidural steroid injections: a scientific evaluation of comparative research for lumbosacral radicular ache. Assessing the superiority of saline versus air for use in the epidural lack of resistance approach: a literature evaluate. A potential evaluation of issues of 10,000 fluoroscopically directed epidural injections. Needle place evaluation in cases of paralysis from transforaminal epidurals: consider alternative approaches to conventional approach. Pathophysiology, analysis and treatment of intermittent claudication in patients with lumbar canal stenosis. Association between peridural scar and recurrent radicular ache after lumbar discectomy: magnetic resonance evaluation. Effect of fluoroscopically guided caudal epidural steroid or native anesthetic injections in the therapy of lumbar disc herniation and radiculitis: a randomized, managed, double blind trial with a two-year follow-up. A randomized, doubleblind, active-control trial of the effectiveness of lumbar interlaminar epidural injections in disc herniation. Transforaminal epidural injections in chronic lumbar disc herniation: a randomized, double-blind, active-control trial. Corticosteroids in periradicular infiltration for radicular ache: a randomised double blind managed trial: one yr outcomes and subgroup analysis. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a potential, randomized, double-blind trial. Effectiveness of transforaminal epidural steroid injection through the use of a preganglionic strategy: a prospective randomized controlled research. The impact of nerve-root injections on the necessity for operative therapy of lumbar radicular ache. Fluoroscopic caudal epidural injections in managing chronic axial low back pain without disc herniation, radiculitis or side joint pain. A randomized, double-blind, active-controlled trial of fluoroscopic lumbar interlaminar epidural injections in persistent axial or discogenic low back pain: outcomes of a 2-year follow-up. Anatomical background of low again pain: variability and degeneration of the lumbar spinal canal and intervertebral disc. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective evaluate. Paraplegia following thoracic and lumbar transforaminal epidural steroid injections: how relevant are particulate steroids Digital subtraction angiography versus real-time fluoroscopy for detection of intravascular penetration previous to epidural steroid injections: meta-analysis of prospective research. Posterolateral percutaneous suctionexcision of herniated lumbar intervertebral discs. Safeguards to prevent neurologic issues after epidural steroid injections: consensus opinions from a multidisciplinary working group and National Organizations. Falco 12 Introduction Pain of thoracic origin has been described to be the bottom of lumbar and cervical regions of the backbone with described prevalence of 5�15%, in comparison with 24�44% of neck ache and 33�56% of low back pain [1�3]. Multiple modalities of remedies have been utilized together with epidural injections [4� 16].
References - Rubesin SE, Herlinger H, DeGaeta L. Interlude: Test Your Skills: inverted Meckel's diverticulum. Radiology 1990; 176:636-644.
- Kirkpatrick UJ, Mossa M, Blann AD, et al: Repeated exercise induces release of soluble P-selectin in patients with intermittent claudication, Thromb Haemost 78:1338-1342, 1997.
- Chua DT, Lo C, Yuen J, et al. A pilot study of pentoxifylline in the treatment of radiation-induced trismus. Am J Clin Oncol 2001;24(4):366-369.
- Tan LB, Chiang CP, Huang CH, et al. Traumatic rupture of the corpus cavernosum. Br J Urol. 1991;68(6):626-628.
- Landolfi R, Steiner M. Ethanol raises prostacyclin in vivo and in vitro. Blood 1984;64:679.
- Krahn M, Lopez De Munain A, Streichenberger N, et al. CAPN3 mutations in patients with idiopathic eosinophilic myositis. Ann Neurol. 2006;59(6):905-911.
- Brochard L, Rauss A, Benito S, et al. Comparison of three methods of gradual withdrawal from ventilator support during weaning from mechanical ventilation. Am J Respir Crit Care Med. 1994;150:896-903.
|