|
Prakashchandra M. Rao, MD, FACS - Clinical Associate Professor of Surgery
- New York Medical College
- New York, New York
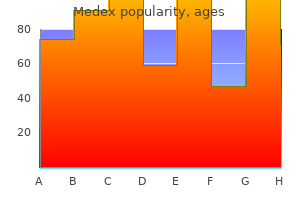
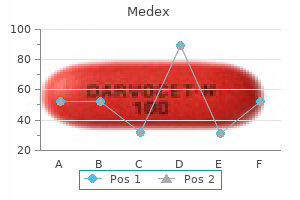
Medex dosages: 5 mg, 1 mg
Medex packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

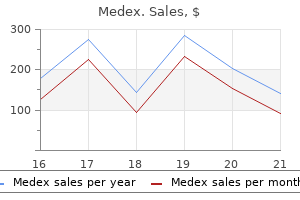
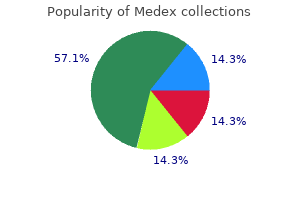
Cheap medex expressThese two sufferers skilled urinary retention after receiving the crossover sling and have been placed on clear intermittent self-catheterization for two weeks hiv infection lymphadenopathy purchase 5mg medex with visa. Comments Patients with multiple prior anti-incontinence procedures characterize a troublesome inhabitants to deal with. The transobturator crossover sling is a comparatively simple different to main operative procedures in girls requiring salvage anti-incontinence surgical procedure. The transobturator strategy allows for the anatomical reconstruction of the natural support of the urethra and on the same time, avoids the scared retropubic house in sufferers with previous failed procedures. The insertion, via the obturator muscle and membrane and the adductor longus muscle aponeurosis, along with the washers, offers good fixation and anatomical reinforcement of the urethropelvic ligaments, reproducing the pure suspension fascia of the urethra. Readjustment can be simply carried out beneath native anesthesia, and just one affected person required readjustment in our first printed collection. Among the advantages of this method, we are ready to mention that it avoids retropubic dissection, could be performed in a short operative time with short hospital keep. We additionally treated two sufferers with neourethral reconstruction because of the urethrovaginal fistula resulting from an advanced labor. These sufferers had no previous antiincontinence process but did have a nonfunctional neourethra after urethral reconstruction. In our first revealed data, this method has proved to be simple to carry out and effective and had minimal issues, which led us to conclude that it was a considerably less-morbid different to bladder neck closure and continent diversion. As the management of failed slings may be a tough situation, spiral sling may be an attractive process, especially in sufferers with regular detrusor perform. We consider that crossover sling supports the midurethra, stopping urethral hypermobility and improving coaptation. This distinctive property offers the surgeon the flexibility to adjust the sling to the desired urethral help stage, thus avoiding urine leakage or retention. This reconstructs the intra-abdominal strain transmission system of regular continent sufferers. The readjustment is made while the patient is standing up and doing the efforts that drives her to incontinence. Rotation both clockwise or counterclockwise elevates or lowers the level of the sling. Surgical approach can current minimal variations according to surgeon desire, however may be standardized as follows. A suprapubic transversal incision of about 3�4 cm within the lower abdomen is made until publicity of the rectus muscle aponeurosis is completed. The anterior vaginal wall is incised for 3�4 cm longitudinally at the stage of the urethrovesical junction and dissected out laterally. The needles are then driven at both sides of the urethra up toward the belly wall, tangent to the posterior facet of the pubic bone, after puncturing via the endopelvic fascia. At this level, cystoscopy is carried out and the needles are repositioned in case of bladder perforation. Polypropylene sutures are then linked to the needles and pulled up till they appear within the belly incision. With the varitensor positioned at 10 cm above the level of the stomach aponeurosis, the sutures are inserted into the varitensor and their ends are knotted to each other. While maintaining the varitensor within the horizontal position, the manipulator is rotated clockwise until the varitensor is positioned three cm above the aponeurosis. The sling support stage can be modified if needed by changing the manipulator and the disconnector under native anesthesia. If urine loss is documented, making 4 full turns on the manipulator and repeating the provocative maneuvers make adjustment of the sling support. After urine loss is resolved, the patient is tested for spontaneous void and postvoid residual. If not, the manipulator is turned 90� in any path, and the disconnector manipulator is well faraway from the varitensor, which stays buried in the fat above the aponeurosis of the rectus muscle as a everlasting regulation mechanism, which can be utilized at anytime as wanted [14]. The sling adjustment is made step-by-step (checking continence every 4 turns of the manipulator). When the affected person is continent, we know that 4 turns earlier than she was incontinent. This permits the surgeon to provide the minimum essential urethral help for that exact affected person under stress and no extra. However, the studied inhabitants was small, follow-up time was considerably brief (mean 12 months) and 62% of sufferers had a earlier unsuccessful anti-incontinence process, however were analyzed altogether together with the relaxation of the cohort who had no previous surgical procedure. Also, goal evaluation of incontinence improvement was not carried out, but only by subjective self-reported patient impression [12]. Authors emphasize the method ought to be beneficial for patients with intrinsic sphincteric deficiency or earlier surgical failure. However, quick follow-up time (average eight months), a small cohort (29 patients), and the dearth of an objective assessment to outline success (selfreported improvement) allow for no definitive conclusion in any respect [15]. There have been 65% of sufferers thought-about cured (use of no pads, small pads, or security napkins) and 20% significantly improved at a imply follow-up of 32 months. No major intraoperative problems occurred and postoperative pain was minimal and successfully managed by oral analgesics [16]. A potential evaluation reported by the Fundacio Puigvert involving 125 patients and a imply follow-up of 38 months reported a remedy price of 87% based mostly on pad test, clinical, and urodynamic standards. Twenty-one patients benefited from readjustment of the sling in the course of the follow-up. The pressure was increased in 17 instances (continent at discharge) as a outcome of recurrence of stress incontinence, and reduced in 4 because of obstruction. More recently, long-term results after 5 years have been offered in a cohort of 30 patients, most of them with extreme intrinsic sphincter deficiency and stuck urethra. In this series, in accordance with goal analysis (pad text and cough stress test), 93% had been thought of cured/improved. Readjustments can be carried out under native 1184 anesthesia at instant or delayed follow-up as needed. However, the evolution of transobturator prosthesis and the emerge of minislings have moved adjustable slings for prohibit subset of sufferers. As the gadgets presented are used in particular conditions these days, the reviews are not often published. So, extra studies are wanted for both methods to corroborate the present information in a sense to provide longer follow-up and extra precise success standards assessments. An integral principle and its methodology for the diagnosis and administration of female urinary incontinence. Safyre sling: Early results of a new tension-adjustable and self-anchoring system for female stress incontinence. Sling Transobturat�rio Reajustavel: Uma abordagem promissora na Incontin�ncia Urinaria de esfor�o.
Buy genuine medexThe kind of delivery is decided by multiple bodily components hiv infection statistics australia order medex 1mg line, including sensation degree, capacity to push with pelvic muscle tissue, measurement of the pelvis, and adaptability around the hips and knees. The more conducive these components are to the birthing process, the extra probably a vaginal delivery can be achieved. It is greatest to deliver in an environment skilled in high-risk pregnancies, with urologist obtainable; integration allows these to be planned appropriately and the sufferers to be acquainted with all elements of their care and the care suppliers. Women with bladder exstrophy have a median gestation at supply of 37 weeks, with 26% at <37 weeks, and customarily have cesarean carried out with general surgeons or urologist present. This has led to an increased collaboration between companies and an increase in both patient and health-care professional satisfaction in care supplied. Models of complete multidisciplinary care for individuals within the United States with genetic issues. Benefit of a specialised multidisciplinary clinic in neurourology and useful urology. Transition care: Future directions in education, health policy, and outcomes research. Adolescent women with disorders of sex growth: A wants evaluation of transitional care. Reproductive outcomes in women with basic bladder exstrophy: An observational cross-sectional study. With this, there are rising calls for positioned on health companies by the challenges the place elderly sufferers might represent a special set of physiological responses that will require a different method to management. This pattern in life expectancy is prone to proceed and the impression of concurrent circumstances, and their therapies will more and more need to be considered as they have an effect on or modify the signs or therapies of incontinence. In essence, these adjustments can current patients and their carers with one or both of two challenges: First, continence is a key concern facing older folks and as such is commonly referred to as one of many geriatric giants [2]. Problems with urinary incontinence improve with age and are significantly common within the hospitalized and institutionalized aged, affecting as a lot as two-thirds of aged inpatients and people in nursing properties [3,4]. Second, health-care professionals dealing particularly with incontinence are going to need to have a better understanding of the issues particular to aging that symbolize necessary cofactors in continence. Currently, regardless of the elevated prevalence and consciousness, many older patients settle for incontinence as part of normal growing older and as such the grievance is underreported. It can be a standard "tipping level" for an individual to transfer into a care home setting. Carer pressure caused by trying to handle relentless incontinence should also not be underestimated [8]. A primary drive of caring for the aged has to be to enhance efforts to elevate basic standards of continence care. This chapter will set out our approach to the multidisciplinary clinic for women with notably advanced multiple issues. To work in partnership with patients, relations, and health-care professionals providing day-today care [9,10] in setting administration plans 5. To feed into different health-care resources as acceptable to enhance overall treatment/management for sufferers Philosophy the service is commissioned as a multidisciplinary service with further funding per consultation offset by the discount in value from different constituent service appointments. By definition, all girls are tertiary referrals as the only route into the clinic is through the care of the aged service or urogynecology service. Consultations happen with both consultants in elderly care and urogynecology, with the support of specialist nurses. All modalities of both providers can be found to all sufferers (albeit modified) so that no patient is excluded from any a part of the service primarily based on age or disability alone. Effects of Aging on the Bladder Through life, the muscle (detrusor) suffers repeated small insults that frequently cause injury and alternative of the muscle fibers with collagen. In addition, there are changes to the nerve supply that are mentioned in additional element in the following. Effects of Aging on the Bladder the mixture of those two events, described earlier in small repeated insults over time during occasions such as being pregnant and childbirth or because of infections or distension, ends in delayed sensation from the nerve adjustments and decreased capacity from the increased stiffness. Over time, cumulative small injuries such throughout pregnancy, infection or distension, cause nerve injury resulting in delayed sensation and decreased capability increase the potential of urgency and urgency incontinence occurring. A further effect of the substitute of the muscle fibers with collagen is lowered efficiency of contraction leading to incomplete emptying and a discount within the useful bladder capacity as a consequence from the failure to empty to completion. These effects are mirrored within the urethra, the place a substitute of muscle with collagen makes the urethra much less compliant. This change is seen as a discount of the maximal urethral closure pressure (potentially growing threat of "failure" of the sphincter) and second a reduction in distensibility throughout voiding decreasing the urinary move price. Retention Management of the situation as early as possible and prior to crisis if achievable is essential to ensure one of the best clinical end result for the woman. Management consists of treating allied conditions recognized to be associated with voiding dysfunction similar to constipation and treating situations that will contribute to complications corresponding to atrophic vaginitis. Acute retention itself, nonetheless, requires catheterization and attempts to enhance voiding with cholinergics have proven disappointing. Specific Effects of Urinary Retention: Physiology and Effects of Distension the bladder is designed as a compliant organ with small stress adjustments for a big change in quantity. Normal storage pressures run between 0 and 10 mmHg with voiding pressures of up to 25 mmHg and pressures above 10 mmHg are sufficient to suppress bladder wall perfusion. If this occurs for extended durations of time, the bladder will endure ischemic changes to the wall. Such a situation may occur when the bladder is over distended and if it is stretched previous the traditional elastic restrict (plastic distension). Effects of Distension Injuries Short-term injuries may be reversible or result in injury, depending on whether or not the bladder tissue stretches past the elastic restrict into plastic deformity. One consequence of that is an alteration in the nerve provide to the bladder, making the muscle extra sensitive to the neurotransmitters [12] within the nerve endings and also a change in the nerve sort. First is that the bladder loses its capacity to empty (although this can often recover with time) [13�15]. The resultant adjustments imply, with time, that the bladder becomes less compliant with filling (reduced capacity) and also has lowered contractility (poorer emptying). The result of these episodes is a substitute of the injured detrusor muscle fibers with collagen. The net impact of that is the bladder begins to lose the elasticity required for compliant distension. Second, the lack of muscle results in a web reduction in contractile drive so the flexibility to empty may cut back. Impact of Voiding Dysfunction Many girls may have suboptimal voiding, but this stays subclinical till symptoms attain the tipping level. First, symptoms of frequency, urgency, poor stream, double voiding, and nocturia develop related to lowered circulate, poor contractility, and delayed/reduced sensation.
Purchase genuine medex lineThe absence of normal hiv infection and aids are you at risk medex 1mg otc, validated definitions prevents comparisons of printed collection from totally different institutions and longitudinal evaluation of a person affected person. A major goal of this report is to introduce a system that may permit the accurate, quantitative description of pelvic support findings in particular person sufferers. This doc is a primary effort toward the establishment of normal, reliable, and validated descriptions of feminine pelvic anatomy and function. The subcommittee acknowledges a necessity for welldesigned reliability studies to consider and validate numerous descriptions and definitions. We have tried to develop pointers that can promote new insights somewhat than current biases. Conditions of the Examination Many variables of examination approach could influence findings in patients with pelvic organ prolapse. It is crucial that the examiner sees and describes the utmost protrusion noted by the person topic throughout her daily activities. Therefore, the criteria for the tip point of the examination and the total improvement of the prolapse must be specified in any report. Suggested standards for demonstration of most prolapse ought to embrace one or all the following: � Any protrusion of the vaginal wall has turn out to be tight during straining by the affected person. For instance, the subject could use a small handheld mirror to visualize the protrusion. Other variables of technique that must be specified during the quantitative description and the ordinal staging of pelvic organ prolapse embrace the following: � the position of the subject. Researchers ought to determine the intra- and interobserver reliability of measurements made with their evaluation techniques before utilizing them as baseline and consequence variables. Manuscript descriptions of assessment methods should include enough element to make positive that other researchers can replicate them precisely. Quantitative Description of Pelvic Organ Position this description system is a tandem profile in that it incorporates a collection of part measurements grouped together in combination, but listed individually in tandem, without being fused into a particular new expression or "grade. Finally, it permits similar judgments as to the end result of surgical repair of prolapse. Definition of Anatomic Landmarks Prolapse must be evaluated by a regular system relative to clearly outlined anatomic factors of reference. There are two kinds of points of reference: mounted reference factors and outlined factors for measurement. Fixed Point of Reference Prolapse must be evaluated relative to a onerous and fast anatomic landmark that can be consistently and exactly recognized. The hymen will be the fixed level of reference used all through this method of quantitative prolapse description. In the sitting or standing position, or in situations with restricted viability as a end result of obesity or restricted capacity for hip abduction, the position of the cervix or the main level of the prolapse relative to the ischial spines could also be measured by palpation. Measurements so obtained should be normalized to the level of the hymen by noting the space between the ischial spines and the plane of the hymen. Because the only construction directly seen to the examiner is the surface of the vagina, anterior prolapse must be mentioned when it comes to a segment of the vaginal wall rather than the organs that lie behind it. Thus, the time period "anterior vaginal wall prolapse" is preferable to "cystocele" or "anterior enterocele" except the organs concerned are identified by ancillary tests. By definition, the range of place of level Aa relative to the hymen is -3 to +3 cm. By definition, level Ba is at -3 cm within the absence of prolapse and would have a constructive value equal to the place of the cuff in ladies with total posthysterectomy vaginal eversion. These factors characterize the most proximal locations of the usually positioned lower reproductive tract. It represents the level of uterosacral ligament attachment to the proximal posterior cervix. It is included as some extent of measurement to differentiate suspensory failure of the uterosacral�cardinal ligament advanced from cervical elongation. When the situation of level C is significantly extra optimistic than the location of level D, that is indicative of cervical elongation, which may be symmetrical or eccentric. Analogous to anterior prolapse, posterior prolapse should be discussed by way of segments of the vaginal wall rather than the organs that lie behind it. Thus, the time period "posterior vaginal wall prolapse" is preferable to "rectocele" or "enterocele" unless the organs involved are recognized by ancillary exams. If small bowel seems to be present within the rectovaginal area, the examiner should touch upon this reality and should clearly describe the idea for this scientific impression. By definition, level Bp is at �3 cm within the absence of prolapse and would have a constructive value equal to the place of the cuff in a woman with complete posthysterectomy vaginal eversion. By definition, the range of place of point Ap relative Other Landmarks and Measurements 1819 the genital hiatus is measured from the center of the exterior urethral meatus to the posterior midline hymen. If the location of the hymen is distorted by a loose band of skin with out underlying muscle or connective tissue, the agency palpable tissue of the perineal physique must be substituted because the posterior margin for this measurement. The perineal body is measured from the posterior margin of the genital hiatus (as just described) to the midanal opening. The total vaginal length is the best depth of the vagina in centimeters when level C or D is lowered to its full normal position. Making and Recording Measurements the place of points Aa, Ba, Ap, Bp, C, and (if applicable) D as regards to the hymen must be measured and recorded. Positions are expressed as centimeters above or proximal to the hymen (negative number) or centimeters below or distal to the hymen (positive number) with the airplane of the hymen being defined as zero (0). The lowest point of the cervix is eight cm above the hymen (-8) and the posterior fornix is 2 cm above this (-10). The vaginal size is 10 cm and the genital hiatus and perineal body measure 2 and three cm, respectively. The fact that the entire vaginal length equals the maximum protrusion reflects the truth that the eversion is total. Point Aa is maximally distal (+3) and the vaginal cuff scar is 2 cm above the hymen (C = -2). The cuff scar has undergone 4 cm of descent since it might be at -6 (the whole vaginal length) if it had been perfectly supported. Point Ap is 2 cm distal to the hymen (+2) and the vaginal cuff scar is 6 cm above the hymen (-6). The cuff has undergone only 2 cm of descent since it will be at -8 (the complete vaginal length) if it were completely supported. Ordinal Staging of Pelvic Organ Prolapse the tandem profile for quantifying prolapse simply described provides a precise description of anatomy for individual patients. While the committee is conscious of the arbitrary nature of an ordinal staging system and the potential biases that it introduces, we conclude that such a system is critical if populations are to be described and compared, if symptoms putatively associated to prolapse are to be evaluated, and if the outcomes of varied remedy options are to be assessed and compared. Stages are assigned in accordance with essentially the most severe portion of the prolapse when the total extent of the protrusion has been demonstrated based on the factors in part "Conditions of the Examination. Points Aa, Ap, Ba, and Bp are all at -3 cm and either point C or D is between -X cm and � (X � 2) cm, the place X is the entire vaginal size in centimeters. The distal portion of the prolapse protrudes to no much less than (X - 2) cm the place X is the entire vaginal length in centimeters.
Buy medex visaLateral stress-free incisions are essential to hiv infection rates in south africa 2015 purchase 1mg medex free shipping release the scar, expose the fistula, and then be succesful of insert the speculum for enough exposure. This can be carried out through the fistula and the catheter ends advanced via the urethra. This is to stop inadvertent injury throughout dissection and inadvertent suturing of the ureter during repair. Wide Mobilization of the Bladder off the Vagina/Cervix/Uterus and Surrounding Tissues the hallmark of successful vesicovaginal fistula surgery is broad mobilization of the bladder, releasing it from scarred attachments to the surrounding constructions and excision of the scar tissue from the bladder and surrounds, so good viable tissue is approximated in the restore. Tension-Free Closure of the Bladder Once the bladder has been efficiently mobilized, the bladder is sutured collectively underneath no rigidity. The bladder is closed with interrupted sutures (2-0 polyglycolic acid) roughly 4 mm aside. To Graft A contentious concern in fistula surgical procedure is whether or not to use an interpositional graft. It has been historically taught this aids healing by bringing a contemporary blood supply to the compromised tissues surrounding the fistula. The commonest graft used is the Martius fibrofatty graft harvested from the labia majora. Other grafts have been described, being of the gracilis muscle, peritoneum, omentum, and broad ligament. One small research did present an elevated success price with utilizing the Martius graft [55]. However, based mostly on a big study accomplished in Ethiopia [56], many fistula surgeons not use grafts routinely and notice comparable success charges to graft interposition. There are situations when a graft could additionally be advantageous, corresponding to for a affected person who has had a number of unsuccessful operations or when the tissues are very thin and fragile, say with the whole reconstruction of a neourethra. To form a Martius graft, an incision is made longitudinally along the bulge of the labia majora. The fats beneath is exposed and a flap of fat developed from anterior to posterior with the pedicle nonetheless being hooked up posteriorly. A tunnel is created into the vagina superficial to the inferior pubic ramus, beneath the bulbocavernosus and vaginal skin. The vaginal and labial skins are repaired, taking precaution to forestall hematoma formation. An anatomical closure may be fairly potential, but a functioning closure is very troublesome. Flaps are then created and sewn over a Foley catheter and this delicate structure is anastomosed to the bladder. A graft is typically placed to assist help and nourish this frail building, a gracilis graft has been described [58], but when a graft is used, the Martius graft is the frequent selection (as talked about earlier). A longitudinal flap is created after dissecting the bladder off the symphysis pubis after which advancing this toward the urethral meatus. The flap sewn right into a tube over a Foley catheter, a graft positioned, and the vagina repaired [59]. This is often not possible with obstetric fistulae as most of these fistulae usually lead to much loss of the bladder tissue; this procedure will thus decrease the dimensions of an already small bladder. When a new urethra is produced from remaining paraurethral tissues, urethral strictures might form in the lengthy term leading to urinary retention and voiding problems. Circumferential Fistulae A circumferential fistula happens against the posterior pubic symphysis. Rectovaginal Fistula the strategies for repair are just like that of the vesicovaginal fistula: flap splitting with extensive mobilization, excision of scar tissue, repair of the fistula underneath no rigidity, and restore of vaginal epithelia. Grafts are rarely used for rectovaginal fistula, but the Martius graft may be employed if a protracted enough pedicle is developed for it to attain the operative web site. Rectovaginal fistulae could be comfortably repaired per vaginum, but some surgeons might prefer to use the abdominal route for the high fistula adhered to the sacral promontory. Diverting colostomies have been used liberally, however in more modern times, fistula surgeons have largely stopped utilizing these with no considerable distinction in outcomes and saving the affected person two additional procedures-opening and shutting the colostomy. A diverting colostomy would nonetheless be advised for very massive (>5 cm in diameter), excessive, and circumferential bowel fistulae, where a breakdown of restore could leak into the peritoneal cavity. Low, large rectovaginal fistulae can nonetheless be safely repaired and not utilizing a colostomy. Note small remaining "tag" of the urethra, then the anterior lip of the bladder, and some 4�5 cm proximally hooked up to the pubic bone. No Vaginal Tissue Remaining About 28% of cases will want some form of vaginoplasty as a result of vaginal skin loss and after restore, dyspareunia and apareunia may result [39,41]. Vaginoplasty could additionally be anything from a simple Fenton-type procedure to release vaginal scarring to reconstruction of a new vagina from tissue flaps, anteriorly from the labia minora and majora and posteriorly with rotational flaps of the gluteal pores and skin. Other options are a neurovascular flap of the tissue from the groin crease or a sigmoid neovagina [62]. Some have used a modified Martius graft with the overlying pores and skin being swung in with the flap. A small randomized managed trial confirmed this to be as efficient when compared to 14 days [63,64]. If a breakdown happens as a end result of poor surgical technique, it usually happens quickly after the operation, within the first few days. Hence, it appears wise to leave the Foley catheter in place at least until this later danger time has passed. This takes meticulous nursing as a full bladder will put stress on the repair site and may even disrupt it. There has been some instances that break later after the repair, after the patient has returned house, which might happen weeks to months after discharge [39,65]. The stools ought to be saved unfastened in instances of rectovaginal fistula with a speedy return to a traditional food plan and use of laxatives. With the second operation, the success fee drops to 79% and with the third, 53% (A. Rates of postoperative incontinence, largely stress urinary incontinence, vary between 5. With time and bladder retraining and strengthening of pelvic flooring muscle tissue, this will improve with time. In northern Nigeria, sufferers have been followed up over a period of 6 months and 15% of closed fistula patients nonetheless have some incontinence at time of final follow-up (K. In a more rural fistula hospital in Ethiopia, 70% returned for follow-up, and 50% of these sufferers discharged with gentle urethral incontinence (leakage of strolling and/or coughing or straining) were cured of their signs with 6 months of conservative remedy. Only 18% of patients suffering with more severe urethral incontinence, leaking with strolling, sitting, and/or mendacity, were improved after 6 months of conservative therapy [39]. The latter group were therefore encouraged to use the urethral plug to hold them dry, and all were inspired to return to hospital for follow-up and a secondary incontinence procedure if it was still wanted [39,66]. A newer however unpublished sequence of nearly one thousand fistula patients with 111 rectal fistulae put the success rate greater at 98%. This is thought mainly to be stress urinary incontinence in type, however detrusor overactivity should additionally play a job. There have been several operations described for ladies suffering urethral incontinence after fistula restore.
Purchase medex without a prescriptionAs the treatment involves dedicated classes with a single clinician new antiviral drugs order 5mg medex otc, the development of that therapeutic relationship can also contribute to improvements in high quality of life. Psychological Therapy Psychological therapies can improve signs with out interacting with pharmacological treatments [96]. Discussion of signs with a supportive health-care skilled who listens and responds appropriately can reduce emotions of isolation and disgrace. Some sufferers want extra formalized psychological interventions, including counseling and cognitive behavioral remedy. Rectal Irrigation Rectal irrigation was initially utilized in scientific practice for children with spina bifida [97]. Indications were prolonged to adults with neurogenic bowel dysfunction after conservative administration had failed [98]. It is now used in a higher diversity of situations corresponding to rectocele, obstructed defecation, and other functional bowel problems [99]. They are designed to be used whereas sitting on the bathroom to avoid accidents when transferring. The larger systems permit irrigation with a cone or balloon catheter, enabling instillation of bigger quantities of water, utilized in patients with sluggish transit constipation or neurological abnormalities (Aquaflush Quick, Qufora, Peristeen). In long-term follow-up of 169 sufferers over 56 months, rectal irrigation was discovered to be efficient in 44% of patients with fecal incontinence and 62% of patients with defecatory issues [24]. Collins and Norton retrospectively assessed 50 consecutive patients utilizing the mini system and found that 62% improved or their signs completely resolved [102]. Absolute contraindications embody stenosis, colorectal cancers, acute diverticulitis, and active inflammatory bowel illness. Most issues reported are minor and include stomach cramps, minor anal bleeding, and leakage of irrigant after completion [99]. Introduction of a medical gadget and administration of water carry a danger of bowel perforation. In a consensus review of best apply, the perforation risk was estimated at 1 per 50,000 and was thought to be noncumulative [103]. It is postulated that stimulation of the tibial nerve in flip stimulates the sacral nerves thus neuromodulating bowel motility and/or sphincter operate. In a pilot examine of 18 sufferers with constipation, the Wexner constipation and Patient Assessment of Constipation Quality of Life scores had been significantly improved after a course of 12 remedies. Subanalysis of the European trial data demonstrated improvement in each colonic transit and skill to evacuate in addition to enchancment in quality of life [113]. Improvement in defecatory frequency with short-term wire placement has been suggested as a great predictor of profitable end result with a everlasting implant [108,112,113]. Complementary Medicine Many sufferers resort to alternative medication in desperation to find a answer to their signs. Patients ought to be suggested to exercise warning when considering different interventions. If a affected person has had earlier appendicectomy or has an atrophic appendix, tubularized ileal or cecal conduits are used. Long-term problems embrace stoma stenosis, leakage, or failure to successfully treat the original symptoms requiring revision, reversal, or conversion to a stoma [7]. Defunctioning Stoma A stoma may be formed as definitive process, as guide to additional treatment, or as salvage from failed different interventions [110]. Colectomy Colectomy should only be considered as a remedy possibility for sufferers with diffuse sluggish colonic transit but normal gastric and small bowel transit [110]. Once a decision to resect has been made, then the following consideration is how a lot to resect. Two studies have reported good results by performing segmental resections or subtotal colectomies primarily based on segmental transit time measurements [42,118]. However, limited subtotal colectomy with cecorectal or ileosigmoid anastomosis is mostly reported as having an inferior useful end result to ileorectal anastomosis [106]. However, an excellent end result may be predicted in patients with gradual transit constipation without impaired evacuation and overt psychological or psychiatric disease [119]. To decide on the most effective remedy options, understanding the pelvic floor anatomy and the DeLancey stage of pelvic organ support (Table sixty three. Transvaginal posterior colporrhaphy was found to have the bottom rate of recurrence of rectocele/enterocele in a Cochrane Review of all rectocele repairs [124]. Dyspareunia has been reported in up to 25% of girls following posterior colporrhaphy. A systematic evaluate of the use of biological supplies in urogynecological surgical procedure has proven that there was no extra benefit to using organic material in rectocele repair [125]. This showed significant enchancment in symptom severity and high quality of life rating. However, 36% skilled complications together with urgency, pain, urinary retention, bleeding, and septic events [126]. Enterocele/Sigmoidocele Enterocele or sigmoidocele occurs as a end result of herniation of small bowel (enterocele) or sigmoid colon (sigmoidocele) through the uterosacral ligament at the vaginal apex into the pouch of Douglas, leading to separation of the rectovaginal septum. This can impede defecation leading to pelvic discomfort and perineal strain with straining [128]. Enteroceles may be repaired transabdominally laparoscopically (ventral mesh rectopexy and sacrocolpopexy) or vaginally in conjunction with pelvic flooring repair (Table 63. Defect Enterocele/sigmoidocele Rectocele Rectal intussusception Supra-anal rectocele Internal Intussusception/Rectal Prolapse Surgically, the rectum is mobilized and returned to its correct anatomical position throughout the pelvis and lots of techniques have been described [120]. In suture rectopexy, the rectum is totally mobilized and sutured to the presacral fascia. In sufferers with redundant loop of sigmoid with preoperative signs of constipation, sigmoid resection could additionally be thought of. Laparoscopic resection rectopexy (Frykman� Goldberg procedure) has been shown to be secure with good long-term end result [129,130]. The use of mesh has been launched on assumption that a overseas physique will produce stronger adhesions and fibrosis than dissection and suture alone. Current literature has proven fashionable nervesparing laparoscopic ventral mesh rectopexy that showed over 50% improvement in the short and medium term [132,133]. Robotic-assisted rectopexy has the advantages of 3D vision, a greater view to determine and spare parasympathetic innervation to the rectum, and having versatile suggestions of instruments for suturing over laparoscopic approach. Recent literature helps security and feasibility of robotic-assisted rectopexy [134]. Perineal procedures are thought of in sufferers with full-thickness rectal prolapse who may not be fit for an belly process and may carry a better recurrence fee [135]. The Altemeier process is transperineal resection of the rectosigmoid, which could be supplied to frail patients with symptomatic massive prolapse. The majority of the patients can be managed conservatively with a multidisciplinary approach (see Chapter 65) in advanced sufferers. Patients with idiopathic constipation could be managed conservatively with out recourse to main surgical interventions. Surgery carries dangers of serious morbidity and affected person choice for surgical intervention have to be carried out with warning.
Fructus Rosae Laevigatae (Cherokee Rosehip). Medex. - Are there any interactions with medications?
- Are there safety concerns?
- How does Cherokee Rosehip work?
- What is Cherokee Rosehip?
- Dosing considerations for Cherokee Rosehip.
- Male sexual dysfunction, gynecologic problems, night sweats, frequent urination, bedwetting, chronic cough, high blood pressure, diarrhea, intestinal swelling (inflammation), and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96865
Cheapest medexUrinary retention might accompany uterine prolapse due to anti viral foods list cheap 5 mg medex concomitant prolapse of the anterior vaginal wall and anatomic kinking of the urethra or obstruction of the bladder neck by the prolapsing cervix. Many women with uterine prolapse report no symptoms till the prolapse approaches the vaginal introitus and beyond. At this stage, widespread complaints embrace a palpable bulge, sensation of vaginal strain or fullness, low back ache, and voiding difficulties. Cervical elongation, which may happen in as a lot as onethird of girls with pelvic prolapse [18], must be assessed with a bimanual examination to palpate the size of cervix protruding, whereas the apical vagina is maximally elevated with the examining fingers suspending every lateral fornix and then visually by using a full bivalve speculum to elevate the vaginal apex to the extent of the ischial spines. The anterior and posterior vaginal compartments ought to be individually and thoroughly assessed using the posterior blade of a bivalve speculum or Sims speculum to retract the other vaginal wall while visualizing the prolapse during straining efforts. In specific, prolapse within the apical and anterior compartments are inclined to usually occur concomitantly, thus reaching passable anterior compartment help that requires consideration to the apex, and vice versa. It is increasingly appreciated that apical help defects symbolize an essential issue underlying cystoceles and also rectoceles [19]. Alternatively, the Baden�Walker "midway" system [22] may be used to describe the place of the cervix relative to the hymenal ring. Using this scale, second-degree uterine prolapse involves a cervix extending to the hymenal ring, third-degree prolapse extends past the hymenal ring, and fourth-degree prolapse represents complete procidentia with no appreciable support remaining. The most severe circumstances, referred to as complete procidentia, contain the uterus fully protruding via the genital hiatus. As surgical therapies turn out to be less invasive and thus more appealing, demand for prolapse operations will more than likely proceed to enhance. Pessary administration stays an option that should be supplied in almost all instances, though clearly, the percentage of ladies selecting this modality has declined in the latest a long time as surgical procedures have become less invasive and extra extensively popularized. Pessaries for uterine prolapse have to present sufficient drainage of cervical secretions and will trigger ulceration, vaginitis, bleeding, and, if left unattended, more severe complications similar to fistula formation with erosion into the bladder or rectum. For uterine prolapse during early being pregnant requiring symptom aid, the Smith� Hodge pessary is the most generally cited; by 20 weeks gestation, nonetheless, uterine prolapse rarely persists as the gravid uterus elevates above the pelvic brim. Although almost any pessary may be tried for uterine prolapse if monitored carefully, dice and donut pessaries ought to be averted with uncommon exception because of their tendency to entice secretions and trigger ulcerations. Topical estrogen is commonly prescribed to postmenopausal girls wearing a pessary to mitigate some of these dangers. In addition to a benign leukorrhea that always happens with pessary use, bacterial vaginosis can be comparatively common and may sometimes require removal of the pessary. Most of the extra severe problems outcome from pessaries which were inadequately monitored [26,27]. Especially patients unable to remove the system on their very own need to be ready for periodic workplace visits in the range of each 6�12 weeks. Most issues can be avoided if the patient removes the pessary overnight, each night time, or several occasions per week. Vaginal and cervical cancers associated with pessary use have been reported but are exceptionally rare [28]. Several surgical approaches can be found, and each must be judged according to how successfully they obtain a successful anatomic end result and an improved high quality of life. Vaginal surgery carries the benefit of its relative security and efficiency, shorter recuperation instances, and in addition the power to efficiently tackle concomitant prolapse defects and stress urinary incontinence. Factors to be thought of embody perioperative danger, present and deliberate reproductive and coital exercise, earlier pelvic reconstructive surgical procedure, and basic well being standing. As the general security of quite lots of surgical approaches has improved, age itself appears to play a lesser role in surgical decision-making. All strategies price considering ought to achieve an efficient suspension of the vaginal apex; this may be completed with or without elimination of the uterus. Moreover, hysterectomy entails purposeful detachment of what stays of these connective tissue helps and structures. In as a lot as 12% of circumstances, hysterectomy performed for prolapse is associated with vaginal vault prolapse and enteroceles later on [22] and in addition may enhance the susceptibility of the anterior compartment to subsequent prolapse defects [29]. An epidemiological examine from Oxford [30] found that the danger of prolapse following hysterectomy was 5. Often, the repair of posthysterectomy prolapse could also be much more challenging than the primary surgical procedure, due to an absence of regular connective tissue structure and strength. On the opposite hand, vaginal hysterectomy is associated with a identified track report and excellent success. Furthermore, removing the uterus eliminates the danger of future interventions for new pathology similar to fibroids, cervical dysplasia, or endometrial hyperplasia. And apart from specific medical reasons, some ladies personally really feel that they "need it out. Hysterectomy with Vaginal Vault Suspension the most typical surgical remedy for uterine prolapse is vaginal hysterectomy adopted by vault suspension, together with repairing any vital concomitant defects of the vagina in the anterior, 1357 posterior, and lateral compartments. It is essential to emphasize that the vault suspension and restoration of anterior and posterior compartment support are the components of this repair that restore pelvic help. In different words, at the moment the hysterectomy is completed and the uterine specimen is removed, the prolapse operation has simply begun. The determination to carry out hysterectomy is commonly more the result of surgical habit and residency training patterns than any scientific evidence. For most practitioners, uterine prolapse is considered an automatic indication for hysterectomy even for circumstances involving no intrauterine pathology, and this interprets into roughly 17% of hysterectomy procedures being carried out for the primary indication of prolapse [31]. Apical suspension at the time of hysterectomy is a critical step, as roughly 12% of women after hysterectomy could develop subsequent vaginal vault prolapse. The procedures most commonly performed throughout hysterectomy embrace uterosacral vaginal vault fixation, sacrospinous or iliococcygeus suspension, and McCall culdoplasty [32]. Uterosacral ligament suspension tends to be performed with various techniques among surgeons, with fixation strengths and results various accordingly. However, in our experience, a fixation sew on the upper one-third of the ligament, near the ischial spine, supplies constant assist and wonderful restoration of vaginal length when every suture is passed by way of the ipsilateral vaginal cuff corner. The McCall culdoplasty is a variation of the uterosacral ligament suspension, wherein the detached uterosacral ligaments are shortened and fixed to the vaginal cuff; this operation often includes closure of the peritoneal cavity by reefing a suture throughout the posterior peritoneum on the rectal reflection. When performing any uterosacral ligament suspension method, intraoperative cystoscopy is critical to demonstrate ureteral patency. Sacrospinous colposuspension has traditionally been described as a unilateral fixation of the vaginal apex, carried out by a posterior (rectocele) method. The vaginal apex is attached, utilizing either permanent or absorbable sutures, to the midportion of the sacrospinous ligament with care, as essentially the most critical issues from this repair are traumas to the pudendal neurovascular structures and inferior gluteal vessels. At our center, although self-limited peripheral nerve accidents have been encountered, pudendal vascular injuries have been utterly averted by adhering to one simple precept: suture into, never over, the ligament. This interprets right into a fixation point situated one to two fingerbreadths directly medial to the ischial spine. Excellent results have been reported for the classical sacrospinous suspension, however the operation additionally has clear limitations. First, the vagina deviates to one side, creating an esthetic however not often useful drawback. Second, the traditional sacrospinous fixation method seems to confer a major risk of recurrent anterior vaginal wall relaxation [37].
Syndromes - Tylenol PM
- Head CT scan
- Never touch electrical appliances while touching faucets or cold water pipes
- While lying down, place a rolled towel under your scrotum.
- Some patients may receive combination therapy
- Sitting for long periods of time
- MRI of the heart
Cheap medex 5 mg with mastercardAt the end of follow-up period hiv infection rate kenya discount 5mg medex, the stress test was unfavorable in all the continent and incontinent patients, and the incontinent group was using one pad per day at the most [5]. Dissection is done to create a 1 cm tunnel lateral to the urethra for the introduction of the needle. First, the needle is superior through the vaginal tunnel until the perforation of pelvic flooring on the level of the midurethra. The proper tension of the sling is adjusted maintaining a Metzenbaum scissors between the urethra and the sling, to prevent undue rigidity. Transobturator Approach (Safyre T) Safyre this a monofilament polypropylene mesh, which is held between two self-anchoring silicone columns that affiliate the universal method with readjustability [6]. Minimal vaginal dissection is carried out laterally towards the inferior ramus of the pubic bone; this minimal dissection avoids injury to the urethral innervations and permits for the passage of the needle and the anchoring columns. Skin punctures are made bilaterally in the genitofemoral folds on the stage of the clitoris. The needle is passed around and beneath the ischiopubic ramus through the pores and skin, obturator membrane, and muscular tissues and eventually out by way of the vaginal incision. This is achieved by introducing the needle vertically in the previously made skin incision till the obturator membrane and muscle are perforated. Next, the needle is introduced to a horizontal place with the tip heading to the surgeons index finger within the vaginal incision. This maneuver permits the surgeon to bring the needle safely to the vaginal incision. Safyre T sling is then hooked by the tip of the needle and dropped at the beforehand made incision. A forceps or scissors is placed between the tape and the urethra throughout intraoperative adjustment, avoiding any rigidity of the tape. For this, a Martius flap is gentile interposed between the neourethra and Safyre T, which was left loosened. In this situation, we used to keep sufferers with a skinny Foley catheter (12 or 14 French) for 21�28 days after which take it out and begin changes if necessary. Readjustment Technique Tightening the process to tighten Safyre could be performed underneath local or spinal anesthesia. As the extremities of the polydimethylsiloxane tails could be simply palpable in the subcutaneous tissue, local anesthesia with lidocaine 1% resolution seems to be the strategy of selection. Usually, the readjustment of just one tail is sufficient, avoiding the risk of significant deviation of the urethral axis. The bladder is crammed with 300 mL saline answer before the procedure, so the patient can be asked to cough and do repeated Valsalva maneuvers to check if leakage occurs. Loosening the process to loosen the Safyre must be done in the first month to avoid fibrosis and may be performed underneath spinal, intravenous, or native anesthesia. The tails are dissected bilaterally, grasped with hemostatic clamps and pulled again, until a Metzenbaum scissors or a right-angle clamp can be comfortably interposed between the mesh and the urethra. Comments the retropubic approach has changing into the preferred method for Safyre implant due to its preferable use in complicated and recurrent patients, but because the transobturator approach avoids the scarred retropubic area in sufferers with previous failed procedures, it must be considered when retropubic space is considered inaccessible. The transmuscular insertion of transobturator Safyre, through the obturator and puborectalis muscular tissues, together with the subcutaneous tunnel, provides good fixation and anatomical reinforcement of the urethropelvic ligaments, reproducing the natural suspension fascia of the urethra. Among some nice benefits of this method, safety, short-operative time, and brief hospital keep must be highlighted [7]. We have previously reported the great outcomes utilizing both the retropubic [4] or transobturator strategy. In our series, readjustments have been performed underneath native anesthesia with nearly 60% of cure or improvement of residual incontinence. Forty patients were randomized for Safyre T transobturator sling or aponeurotic retropubic sling. The transobturator group offered lesser problems price than the retropubic group. Authors concluded that the transobturator and the aponeurotic slings techniques have been equally efficient, however the transobturator sling has shown fewer problems and lesser surgical time than the aponeurotic sling [8]. Although retention can subside after 4 weeks postoperatively, we advise the loosening procedure inside this period in order to avoid fibrotic reaction around the sling and to allow for the patients to resume them as soon as potential. Safyre self-anchoring system is exclusive as far as postoperative readjustability is worried. The process is minimally invasive and no giant abdominal incision is required for harvesting fascia. Sling fixation to the aponeurosis of the stomach rectus muscle as in classical slings is also pointless. Its late adjustments of sling pressure are attainable in patients presenting persistent incontinence or urinary retention, avoiding main surgeries corresponding to urethrolysis or the need for another sling insertion. The readjustment price in our sequence was 10% leading to successful of 40% of the circumstances and enchancment in 20% of this subset of patients [5]. It is our understanding that sling tightening in incontinent sufferers may be carried out at any time; on the opposite hand, loosening the sling should be accomplished between four and 6 weeks at the newest to avoid bladder outlet obstruction attributable to fibrosis. A Martius flap is interposed between the neourethra and Safyre to stop neourethral erosion. Safyre was left loosened and adjustment can be performed after 30�40 days postoperative, if necessary. Regarding issues, there have been no vascular, bowel, or obturator plexus accidents. No patients reported voiding symptoms after 4 weeks of the procedure, confirming the low "de novo" detrusor overactivity price. Safyre combines the benefits of the transobturator method with readjustability and could additionally be a beautiful surgical various. These patients have misplaced completely the urethral sphincteric function and the urethra acts solely as a conduct. The subset of patients might benefit from 1177 undergoing a extra obstructive sling which could be mounted with more pressure than normally required or ideally through the use of a normal sling [5]. In this scenario, sufferers should be knowledgeable about the potential need for postoperative intermittent self-catheterization and urinary symptoms that will happen subsequently. We first described transobturator crossover readjustable sling for treating these complicated cases [9]. This hybrid sling consists of a monofilament polypropylene mesh that acts as a urethral help held between two self-anchoring columns that are made of an implant grade polydimethylsiloxane polymer. The equipment has additionally two delicate and radiopaque silicone washers that not only improve fixation when rigidity is critical but additionally enable for straightforward identification should readjustment become essential. The vaginal wall is dissected from the underlying periurethral fascia, bilaterally to the inferior ramus of the pubic bone. The urethra is recognized and a right angle clamp is passed between the pubic bone and the urethra, exiting on the opposite facet. One of the extremities of the sling is grasped and brought about behind the urethra to the contralateral side.
Order 1 mg medex mastercardLess widespread causes include superior pelvic cancer; sexual trauma acute hiv infection how long does it last buy medex 5 mg with mastercard, particularly in young undeveloped ladies; infections, similar to tuberculosis of the bladder; schistosoma; and lymphogranuloma venereum. There have been quite a few epidemiological studies of obstetric fistula patients from numerous parts of the globe. Interestingly, a number of studies have shown these women to be quick, typically lower than one hundred fifty cm in Nigeria [5], India [6], Ethiopia [7], and Niger [8]. The girls are largely uneducated, greater than 92% having had no formal schooling [4,10,11]. A latest study showed that girls struggling fistula in Tanzania and Sierra Leone have a much narrower intertuberous house as in comparability with those women delivering usually and also reconfirmed a brief stature among fistula sufferers, however the latter was a weak predictor of fistula formation [12]. If their age is requested and the answer relied upon, a 42% are aged less than 20, with 65% being lower than 25 years old [4]. The majority have had home deliveries with no skilled attendant present and usually greater than 50% have been divorced by their husbands because of their offenses [4]. This was confirmed in a research evaluating fistula sufferers with and without circumcision in northern Ethiopia. There was no distinction between the presentation, type of injury, and outcomes when comparing 255 obstetric fistula patients with type 1 and 2 circumcision and 237 obstetric fistula sufferers with out circumcision. During labor, a traditional well being attendant may reduce the circumcision open, cutting anteriorly, damaging the urethra, bladder neck, and bladder base. It seems cheap to assume that because grownup height and sexual maturity are reached earlier than the completion of pelvic development, early marriage and, therefore, being pregnant might result in a rise in obstructed labor and, hence, obstetric fistula [16]. The ratio of primiparous to multiparous is comparable in areas not so famend for early marriage. Unfortunately, early marriage may end up in traumatic fistula, if the husband must enlarge the vagina of a younger woman to enable intercourse to happen. This is usually accomplished, once more by a traditional healer chopping open the vaginal tissues anteriorly and sometimes damaging the urethra and/or bladder in the course of. This is just like a "gishiri" reduce performed in some areas as a traditional remedy in some areas for quite so much of gynecological ills [10]. There have been few population-based studies to determine the scope of the problem [17]. A large hospital-based examine of over 22,000 sufferers gave the incidence of obstetric fistula as 0. Knowing the vast majority of ladies within the growing world deliver of their villages and never in a hospital, the true incidence was thought to be higher. Using this determine, there are in all probability between 50,000 to a hundred,000 new instances of obstetric fistula occurring internationally annually and about 2 million girls affected by this situation all through the world [19]. Others have taken further calculations equating the obstetric fistula rate with maternal mortality. Danso, understanding that for each maternal demise, there are at least 30 girls affected by morbidity, considered certainly one of which may be an obstetric fistula. This would make about 500,000 new instances of obstetric fistula worldwide every year [3]. Recent research trace that this might be overestimated, and a meta-analysis accomplished in 2013 means that the prevalence is zero. Rarely, if the fistula may be very small, she can describe signs more like stress urinary incontinence, but leaking from the vagina rather than the urethra. If she has sustained similar accidents to the posterior compartment, she is also rendered incontinent of feces and flatus per vagina. It is straightforward to consider the obstetric fistula as merely only a gap in the vagina to the bladder and maybe the rectum. Primary Conditions Vesicovaginal Fistula the extent of impaction during labor determines the location of damage. The urethra is injured in 28% of instances with 5% of sufferers in Ethiopia having the urethra utterly destroyed [21]. This has prognostic indications as the mechanisms for continence in the female have been destroyed [17,23,24]. Ureteric Injury In a small variety of obstetric fistula circumstances, the lower part of the ureter may be concerned. The whole ureterovesical junction is necrosed and sloughed away, leaving the vesicovaginal fistula with the ureter draining outside of the bladder straight into the vagina. It is changing into more frequent to see isolated ureterovaginal fistulae after cesarean section or cesarean hysterectomy, more commonly on the left, and these are iatrogenic, occurring at the time of operative delivery [2,25]. Rectovaginal Injuries A rectovaginal fistula occurs if the presenting part is impacted in opposition to the sacrum during labor, inflicting ischemic necrosis of the rectovaginal septum. It has varied reported prevalence and seems to range geographically, ranging between 6% (B. If current, it usually occurs at the facet of a vesicovaginal fistula, rarely presenting in isolation [4]. The standing of the anal sphincter ought to at all times be noted as there could additionally be residual flatal or fecal incontinence even after restore [26]. Muscles the muscles of the pelvic basin are sometimes affected by a neuropathy, immediately weakened by the ischemic course of or even fully destroyed. A recent ultrasound examine of the levator muscle complex in obstetric fistula patients confirmed little muscle loss and little denervation [27], but definitely in extensive injuries, an "empty pelvis" is all that continues to be. Bones A series by Cockshott performed x-rays on 312 girls with obstetric fistula and located that 32% had some x-ray abnormality, ranging from bony resorption, bony spurs, obliteration or separation of the symphysis pubis [28]. Nerves It has been quoted that between 20% and 65% of obstetric fistula, sufferers will have some type of peroneal neuropathy manifesting as bilateral or unilateral foot drop [21,29]. There are at present three theories as to its etiology: a prolapsed intervertebral disc, direct compression of the fetus on the lumbosacral trunk throughout labor, or impingement of the frequent peroneal nerve as it transverses the pinnacle of fibula while the patient squats for prolonged durations throughout labor [30,31]. Waaldjik and Elkins commented that the majority patients do improve with time with 13% still displaying some signs at 2 years [29]. Secondary Conditions Social Consequences the implications of full incontinence for a girl within the developing world, the place the status of girls is usually low, are far reaching. Over half are divorced by their husbands who really feel that the affected woman is now unable to fulfill her marital duties and unable to bare youngsters [4]. Her incontinence has other penalties as she is now in urine-soaked garments, unable to clean herself or her apparel. Mental Health It is changing into more apparent that psychological well being issues in obstetric fistula patients are a big illness burden [32�36]. Similarly, in Kenya, 17% of sufferers had suicidal ideations earlier than receiving therapy, 73% were depressed, and 26% severely depressed [35]. If, nonetheless, the affected person is cured fully by the operation and has no residual incontinence, the share screening optimistic returns to the background positive rate from the final inhabitants [33,36]. Malnutrition Malnutrition results from isolation as the patient could also be fed and cared for inadequately by a relative in a small room or hut. Upper Renal Tract Damage One examine from Nigeria taking a look at intravenous pyelograms in girls with fistula revealed 49% of patients sustained higher renal tract injury.
Order medex overnight deliveryExtravasation of saline or urine into the abdomen confirms the presence of a cystotomy antiviral vitamins for herpes order medex 1 mg visa. During benign gynecological surgical procedure, the ureter may be injured along its path from the renal pelvis to the trigone of the bladder. A frequent web site of ureteral injury during abdominal hysterectomy is on the pelvic brim the place the ureter lies beneath the infundibulopelvic ligament [13]. A second frequent web site of harm (at danger throughout uterosacral ligament suspension) is the lateral pelvic side wall next to the uterosacral ligaments, often thickened in circumstances of endometriosis [41]. A third location (injury can occur during complete hysterectomy) is on the stage of the cervical internal os, the place the uterine artery crosses the ureter over the iliac arteries, also identified as the cardinal ligament [13,14]. Additionally, the ureter can be compromised (during excision of the cervix and vaginal cuff or even throughout closure of the vaginal cuff) the place it passes anteriorly and lateral to the fornix of the vagina just as it enters the trigone of the bladder [13]. In order to finest keep away from ureteral injury during hysterectomy, the surgeon ought to identify the ureter at each step within the procedure. Common websites of harm that advantage additional warning embrace ligation of ovarian vessels and uterine vessels and with closure of the vaginal cuff. Isolating the uterine vessels with meticulous dissection aids in excluding the ureter from the vascular clamp. When putting any clamp, the surgeons ought to only include vessels and must examine that the ureter is excluded before applying the clamp. Once the uterine vessels are ligated, the ureter ought to then fall inferior and lateral to the pedicle. Subsequent bites should solely be taken medial to this pedicle to keep away from any ureteral injury. In addition, care should be taken to mobilize the bladder off the anterior cervix allowing the ureters to descend with the bladder. If urinary tract damage is recognized intraoperatively, it should be immediately repaired so as to stop infection, urinary leakage, or threat of fistula formation. All sufferers present process gynecological surgery should have sterile urine and should obtain surgical web site an infection prophylaxis. There is a basic lack of knowledge to counsel any advantage to additional antibiotic protection following restore of intraoperative decrease urinary tract damage. During the postoperative period, fever, chemical peritonitis, stomach or flank pain, leukocytosis, anuria, urinary leakage from wound, hydronephrosis, or hematuria might signify bladder or ureteral injury. With injuries to the distal ureter, ureteroneocystostomy is typically favored over end-to-end ureteroureterostomy restore. Ureteroneocystostomy bypasses the site of injury and permits for easy proximal dissection and excision of any devascularized section, eliminating any need for difficult dissection of the distal ureter [42]. Success charges are close to 100 percent with ureteral 1757 reimplantation [43�45], and the risk of ureteral obstruction is minimized by avoiding an antirefluxing anastomosis. On the opposite hand, ureteroureterostomy has an unacceptably excessive rate of stricture, because of embarrassment of the distal ureteral blood supply that usually happens with the damage. The location of the injury and the degree of ureteral and bladder mobility will dictate the method of implantation. While a distal ureteral injury is amenable to easy ureteral reimplantation, in the setting of a extra proximal damage, a ureteroneocystostomy could also be aided by a psoas bladder hitch to decrease anastomotic rigidity [44]. A Boari flap substitute of the distal ureter is indicated when the obstructive section lies even more proximally [45,46]. With high or long ureteral strictures, a more advanced reconstruction similar to transureteroureterostomy, renal descensus, renal autotransplantation, or ileoureterocystoplasty could also be necessary. Nephrectomy ought to be undertaken as a last resort and solely within the setting of a traditional contralateral renal unit [45,46]. In the rare instance of a midureteral or proximal ureteral transection, ureteroureterostomy would be preferred, however only if the anastomosis may be widely spatulated and tension-free. Indwelling double pigtail stents are positioned and normally left in place for no less than 6 weeks. Closed suction drains ought to be left in place after repairs and monitored for urine leakage. Postoperative antibiotics are sometimes not indicated if the preoperative urinalysis was adverse. Anticholinergic medicine might assist to scale back complaints of painful bladder spasm. Fistulization occurs when a ureteral leak persists and the urinoma establishes a communication with the vaginal cuff. Any unexplained abdominal or flank ache or findings of costovertebral angle tenderness ought to alert the surgeon to the chance of a ureteral injury. The typical presentation is one of sudden onset leakage from the vagina 1 to 4 weeks postoperatively. In a female with vaginal leakage after pelvic surgical procedure, a double dye test might differentiate between vesicovaginal and ureterovaginal fistulae [48]. The vagina is packed and methylene blue is given intravenously, whereas purple carmine is instilled intravesically. The vaginal pack will stain red if a vesicovaginal fistula is present and blue if a ureterovaginal fistula is present. Alternatively, oral pyridium can be given several hours prior to bladder instillation with methylene blue, with orange staining or blue staining confirming a ureterovaginal or vesicovaginal fistula, respectively. Management should urgently deal with any ureteral obstruction with an inside ureteral stent if potential, or a percutaneous nephrostomy, with definitive repair through open or laparoscopic surgical repair, and even nephrectomy. Controversy exists regarding timing of repair, with some surgeons performing immediate, while others advocate early higher tract drainage adopted be delayed ureteral restore [50�55]. While the surgery may be somewhat less cumbersome by waiting a number of months for inflammation to subside, the outcomes for early versus delayed restore are comparable [56]. Retrograde ureteropyelography is really helpful and could also be diagnostic and therapeutic if a stent could be handed. Should a stent be positioned to bypass the fistula, spontaneous therapeutic is in all probability going, but should still require additional intervention [57,58]. If retrograde ureteral stenting is unsuccessful, antegrade percutaneous nephrostomy is beneficial. With decompression of the kidney, the obstruction is relieved, and entry for antegrade ureteral stenting is achieved. If neither anterograde nor retrograde ureteral entry is profitable, open surgical repair is indicated. Meticulous surgical technique and familiarity with pelvic anatomy are important for every gynecological surgical procedure. Intraoperative discovery of bladder or ureteral damage can be achieved with careful inspection, cystoscopy, or from concern because of proximity of suture, ligation, or thermal use. Repair ought to at all times be attempted at time of recognition to decrease any future morbidity, issues, and urogenital fistula. Patients who present postoperatively with fever, stomach or flank ache, vomiting, ileus, low urine output or leakage of urine from the vagina, or incision raise concern for lower urinary tract harm. Repair of ureteral accidents should start with an try at retrograde or antegrade stenting, and if that fails, advanced surgical restore or reconstruction may be needed.
References - Kimoto S, et al: Ultrasonic tomography of the liver and detection of heart atrial septal defect with the aid of ultrasonic intravenous probes, Ultrasonics 2:82, 1964.
- Prochaska JO. Changing for Good. New York, NY: Avon Books, 1994.
- Babb RR. Radiation proctitis: a review. Am J Gastroenterol. 1996;91(7):1309-1311.
- Donaldson JF, Tait C, Rad M, et al: Obstructive uropathy and vesicovaginal fistula secondary to a retained sex toy in the vagina, J Sex Med 11(10):2595n 2600, 2014.
- Pierson DJ, Horton CA, Bates PW. Persistent bronchopleural air leak during mechanical ventilation. A review of 39 cases. Chest 1986; 90: 321-323.
- Lerman BB, Wesley RC, Belardinelli L. Electrophysiologic effects of dipyridamole on atrioventricular nodal conduction and supraventricular tachycardia: role of endogenous adenosine. Circulation 1989;80(6):1536-1543.
- Abrahamson PE, Hall SA, Feudjo-Tepie M, et al. The incidence of idiopathic thrombocytopenic purpura among adults: a population-based study and literature review. Eur J Haematol. 2009;83(2):83-89.
- Forster C, Clark HB, Ross ME, et al. Inducible nitric oxide synthase expression in human cerebral infarcts. Acta Neuropathol 1999;97:215-20.
|